Partial Hysterectomy vs Total
Hysterectomy is probably after cesarean section, the surgery most often performed by gynecologists. Just as important as knowing how to do it is knowing when to indicate it.
Today we are going to talk about hysterectomy in general and we are going to give a few hints about the considerations that we have to have before performing a hysterectomy. When to do it, if a prophylactic oophorectomy should be done or not if the cuff should be suspended if a total or partial hysterectomy should be done.
The most important aspect of a hysterectomy procedure is making a good surgical indication.
It is probably a surgery that during the last decades, has been over indicated. And more hysterectomies have been performed over many years than were necessary.
In recent years, gynecologists are being more selective and indicated hysterectomies when they are truly necessary.
In many cases, they opt for techniques that are less invasive, less aggressive, or can even maintain an expectant attitude.
In some cases, some of the most frequent indications for a hysterectomy are uterine myomatosis. Although we already know that we are increasingly restrictive or more selective when it comes to indicating it. Cancer has already been of the cervix, endometrium, myometrium (a uterine sarcoma), or ovarian cancer.
A hysterectomy is also performed if there is hyperplasia, especially if it is with atypia, hyperplasia without atypia in principle, they do not need a hysterectomy. When there is heavy menstrual bleeding that is refractory to all previous treatments and sometimes, endometriosis may end up requiring a hysterectomy, although this is not usual.
Another very common indication for hysterectomy is uterine prolapse, apical prolapse. In this case, the hysterectomy is usually done vaginally.
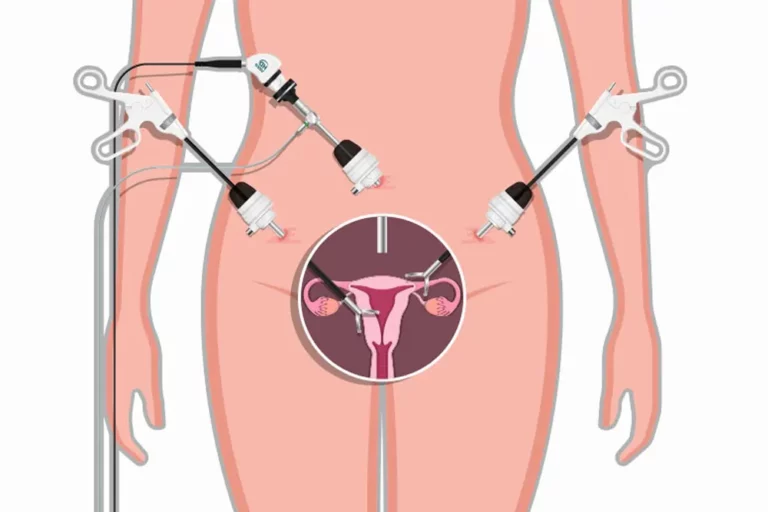
Hysterectomy can be performed vaginally or abdominally.
Within the abdominal approach, we have three possibilities. It can be done by open incision, which is the classic approach and probably the most widely used yet. It can be done laparoscopically or it can be done with an alternative to a variant of the laparoscopic which is robotic surgery.
In general, the laparoscopic and the vaginal approach are the best tolerated. However, they are not always technically possible and there are times when we have to resort to open abdominal surgery to perform the hysterectomy. In addition, open surgery, abdominal surgery, is resource surgery, that is, when other routes cannot be used, the abdominal approach is used. Therefore, every gynecologist must be able to perform an open abdominal hysterectomy.
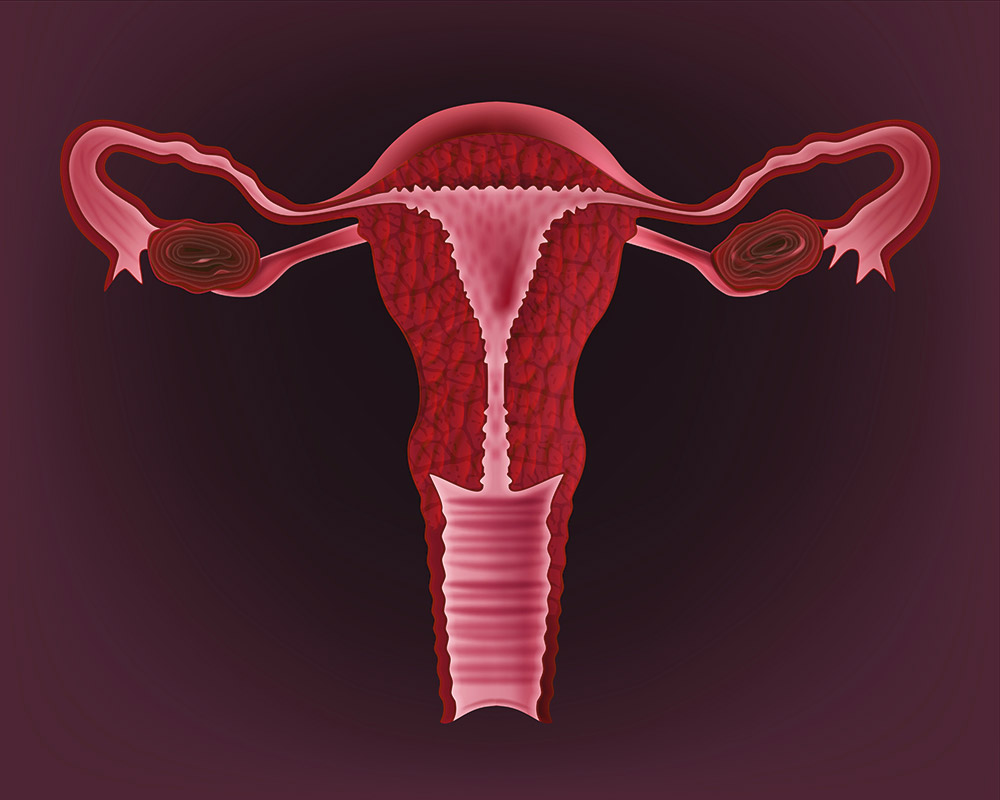
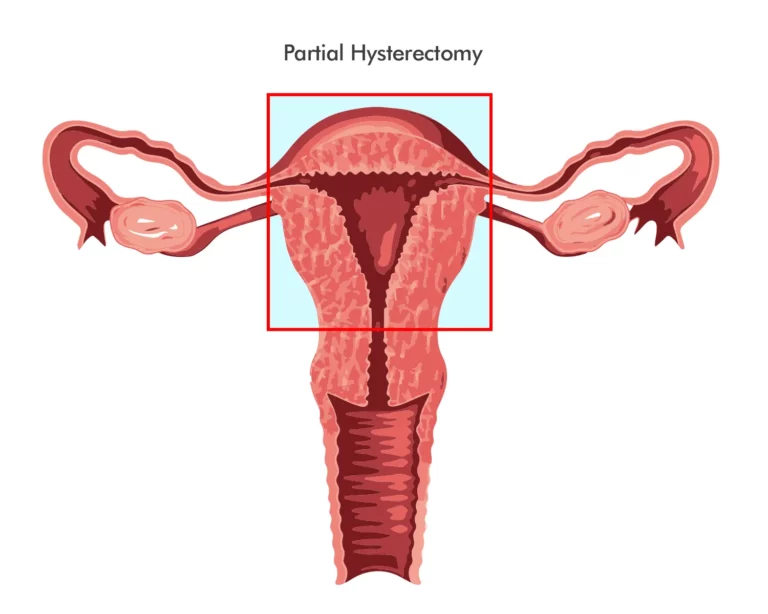
Regarding the decision to perform a total or partial hysterectomy, it is a very controversial issue on which not everyone agrees. The difference is that in the total hysterectomy the entire uterus is removed, while in the partial or subtotal hysterectomy we will leave the cervix or part of it.
The main benefit of performing a total hysterectomy, that is, including the cervix, is that we will not need to perform subsequent cytology because we eliminate the possibility of cervical cancer appearing.
The main benefit of performing a total hysterectomy, that is, including the cervix, is that we will not need to perform subsequent cytology because we eliminate the possibility of cervical cancer appearing.
In general, total hysterectomy is the most widespread technique except in cases that are technically complicated.
In the case of a total hysterectomy, some type of vaginal vault plication appears beneficial to reduce the risk or rate of vaginal vault prolapse in the future.
Partial hysterectomy, in other words, maintaining the cervix, reduces surgical time and probably also reduces the risk of complications at the level of the bladder, ureters, and possibly also at the level of the rectum.
However, although some authors defend it, it has not been proven that subtotal hysterectomy reduces the risk of prolapse in the future.
Nor does it seem that the indication for a total or subtotal hysterectomy has an impact on sexual function, however, there is no consensus in this regard because for some authors the innervation that comes from the cardinal ligaments, that is, from the cervical ligaments, as well as the secretion at the level of the cervix does have some importance when having sexual intercourse. Therefore, as there is no definite consensus that it is better to do a total hysterectomy than a partial hysterectomy in general, the choice of surgeon is left to the choice of the patient and the decision to remove or not remove the cervix.
The decision to remove or not remove the ovaries prophylactically to eliminate the risk of ovarian cancer is also a very controversial issue when we perform a hysterectomy. Historically until a few years ago all women over 40 years old, whenever a hysterectomy was performed, the adnexa were also removed, that is, the ovaries and tubes to eliminate the risk of ovarian cancer and also theoretically to reduce the risk of breast cancer. Although this has never been proven.
In women who are not at increased risk of breast cancer, prophylactic adnexectomy does not appear to have any benefit. For its part, the risk of ovarian cancer in total numbers is quite low because the incidence of ovarian cancer is itself quite low. As long as we are not faced with a patient with a familial inheritance syndrome that increases the risk of ovarian cancer. In addition, as we will see later, the hysterectomy itself seems to reduce the risk of ovarian cancer in the future. So should the ovaries of patients who have a hysterectomy be removed? Well, it is a controversial issue because adnexectomy, removing two ovaries is not a decision that is totally risk-free.
If we perform an oophorectomy, that is, removing the ovaries in a patient before menopause, we will be inducing surgical menopause, therefore we will be advancing the age of menopause. In addition, contrary to what was believed, the ovaries after menopause also have a certain function when it comes to protecting cardiovascular risk and protecting against osteoporosis. Therefore, removing the ovaries from an impatient person after menopause seems to increase the cardiovascular risk, osteoporosis and it has even been seen that it can increase the risk of chronic kidney disease, cognitive impairment, parkinsonism, and that it can alter sexual function.
In conclusion, it seems that prophylactic oophorectomy, as reflected in the latest guidelines, is not justified in patients under 65 years of age. Because if we put a balance between the mortality caused by ovarian cancer, which is rare cancer and the increase in mortality produced in patients under 65 who underwent a hysterectomy, it seems that the balance tends to increase the risk in women who had an oophorectomy. Therefore, in patients who are under 65 years of age in principle, if there are no other risks, the ovaries should be preserved. However, in women who have an increased risk of ovarian cancer, it would be necessary to individualize based on age and the risk of suffering from this cancer.
There are many other ways to lower the risk of developing ovarian cancer. We have already stated that hysterectomy appears to decrease the likelihood of developing ovarian cancer. In addition, it has been seen that if we perform a salpingectomy, that is, we remove only the tubes and preserve the ovaries. This can lower the chance of developing ovarian cancer in the future by as much as 50%. Therefore, and again as reflected in the latest guidelines, it does seem indicated to perform a prophylactic bilateral salpingectomy in women who undergo a hysterectomy.
When a hysterectomy is to be performed, a prophylactic thrombus is indicated in patients without risk factors and it seems that mechanical prophylaxis with compression stockings as early mobilization may be sufficient. However, in general, what is most recommended is drug prophylaxis thrombus.
Antibiotic prophylaxis prior to surgery is also indicated in all patients who are to receive a hysterectomy, thus reducing the risk of infections.
When an extrafascial hysterectomy is performed, the uterus sacral ligaments are cut and therefore the risk of a vaginal vault prolapse will be increased. Therefore, whenever an extrafascial total hysterectomy is performed, some type of plication will have to be performed to prevent the vaginal vault from prolapsing in subsequent years.
To avoid this prolapse, a total intrafascial hysterectomy can be performed with that we will preserve the cardinal ligament or at least in part and we will preserve the uterosacral ligaments. It is also possible to reduce the risk of prolapse by incorporating the uterus sacral ligaments into the vaginal cuff that has been opened and when closing this vaginal cuff it is incorporated into the sutures of the uterine sacral ligaments and these will slightly tighten the vaginal cuff, reducing the risk of prolapse in the future.
Neither of these two techniques has been shown to be better than the other in preventing future prolapse, therefore this decision will be left to the surgeon’s choice.
Regarding post-operative care, although early mobilization is always recommended, which is already known to benefit a lot, we must recommend that the patient avoid efforts and above all avoid lifting weights for four or six weeks after surgery. We must also recommend that patients do not have penetrative intercourse until we have verified that the vaginal cuff has completely closed this in clear total hysterectomies.