Partial Hysterectomy: What is, Procedure and Recovery Explained
A partial hysterectomy is a medical procedure in which the uterus is removed but the cervix is kept in place. This surgery can be carried out using a variety of techniques, including laparoscopic, vaginal, or abdominal procedures, and it may be advised for a number of different reasons. In this article, we’ll go over what a partial hysterectomy is, the many forms, the justifications behind it, how it’s carried out, any potential side effects, recovery and alternatives.
Types of Hysterectomy Surgery
Depending on which portions of the female reproductive system are removed, hysterectomy surgery can be divided into three primary types:
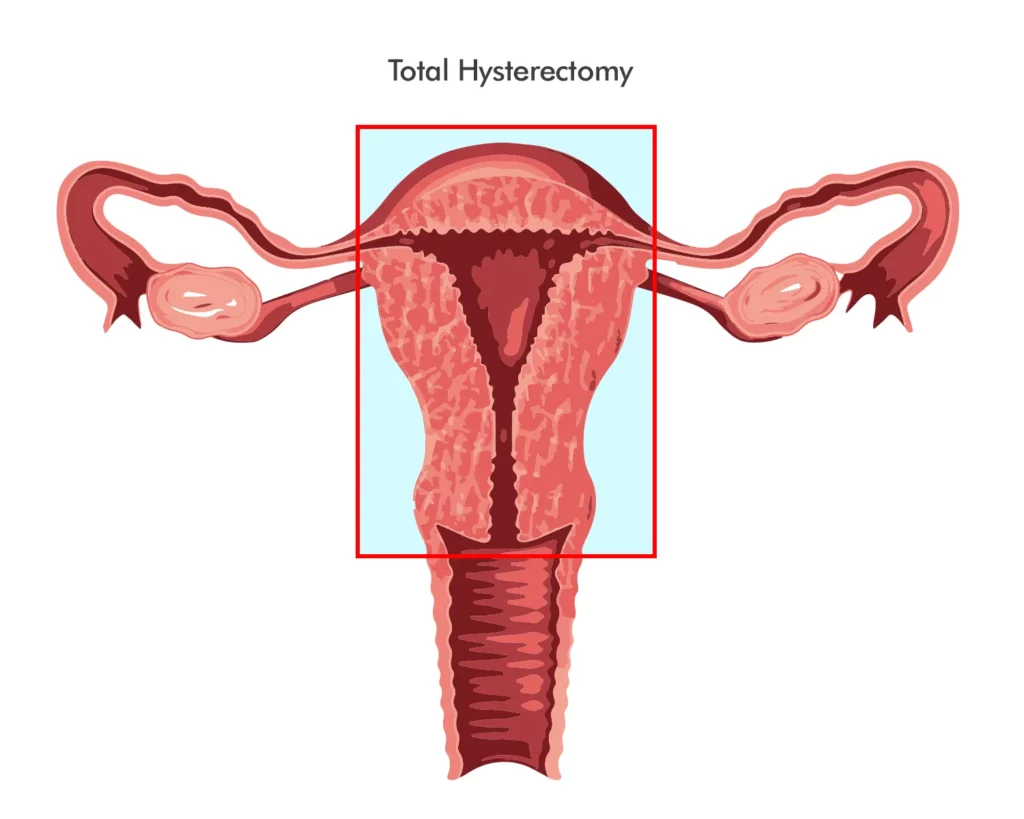
Total hysterectomy
This type of hysterectomy entails the complete removal of the uterus, including the cervix. The most prevalent type of hysterectomy is a total hysterectomy, which can be performed via abdominal, vaginal, or laparoscopic surgery.
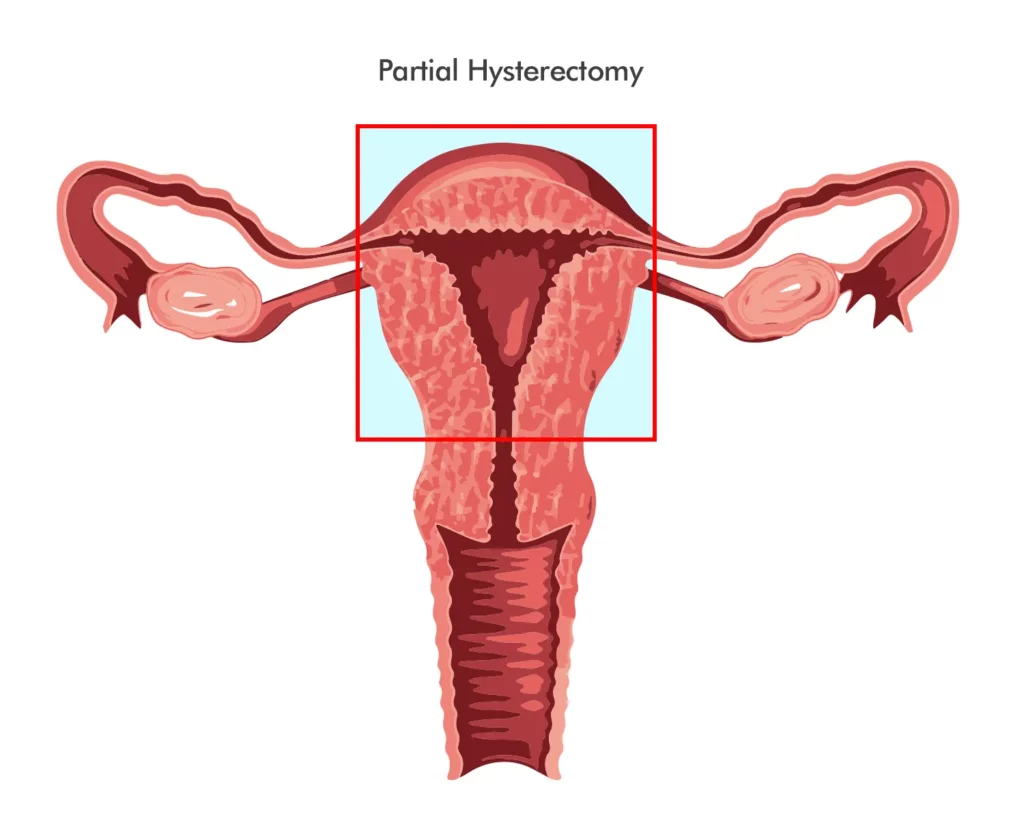
Partial hysterectomy
This form of hysterectomy consists of the removal of the upper portion of the uterus while keeping the cervix intact. Subtotal hysterectomy is less common than total hysterectomy and may offer certain benefits, including retaining sexual function and lowering the risk of cervical cancer.
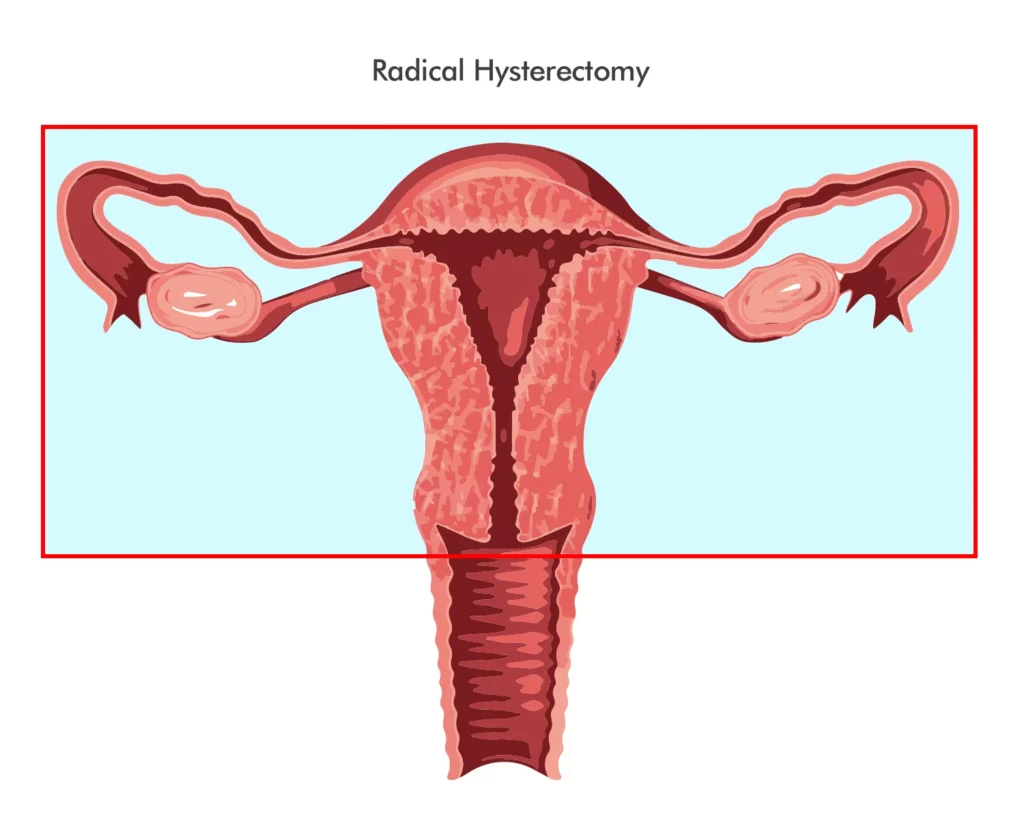
Radical hysterectomy
This form of hysterectomy involves the complete removal of the uterus, cervix, and surrounding tissues, including the ovaries, fallopian tubes, and lymph nodes. Generally speaking, women with severe or aggressive forms of gynecologic cancer undergo a radical hysterectomy.
Each type of hysterectomy surgery has its own benefits and risks, which should be discussed with your gynecologist or surgeon before making a decision.
How a Partial Hysterectomy is performed
It is possible to conduct a partial hysterectomy laparoscopically, vaginally, or abdominally. Depending on the patient’s unique circumstances and the surgeon’s preference, a particular technique may be employed.
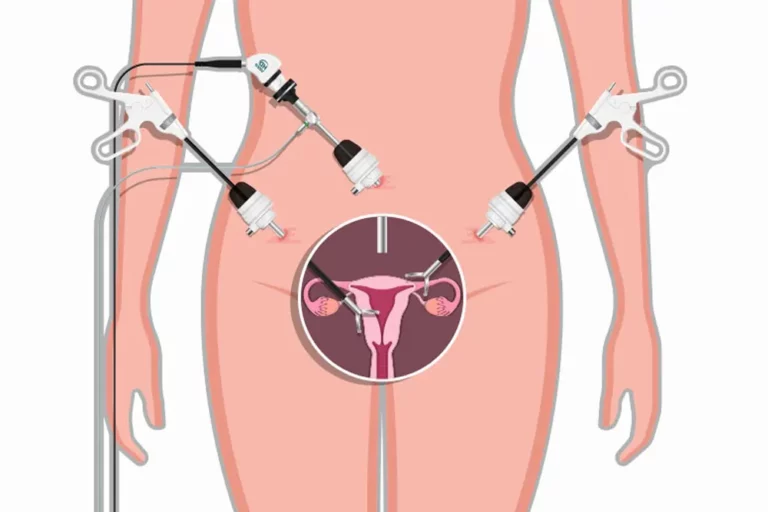
Laparoscopic
During a laparoscopic partial hysterectomy, the surgeon makes small incisions in the abdomen and inserts a laparoscope to view the uterus and surrounding organs. The uterus is then removed using tiny devices while the cervix remains intact.
Vaginal
There are no exterior incisions created when performing a vaginal partial hysterectomy. The uterus is extracted through the vagina while the cervix remains intact.
Abdominal
A significant abdominal incision is used to execute an abdominal partial hysterectomy. The surgeon can more easily access the uterus and the surrounding organs using this technique, which is employed for more complicated patients.
Reasons for having this procedure
- Fibroids
Fibroids are noncancerous uterine growths that can result in heavy bleeding, discomfort and other symptoms. - Endometriosis
With endometriosis, the tissue that borders the uterus expands outside of it, leading to discomfort, infertility and other issues. - Adenomyosis
Adenomyosis is a disorder that causes pain , excessive bleeding and other symptoms when the tissue that borders the uterus develops into the muscular wall of the uterus. - Uterine prolapse
When the uterus prolapses into the vagina, it can be uncomfortable and lead to incontinence. - Cancer
For some cancers, such as endometrial or cervical cancer, partial hysterectomy may be suggested as a course of treatment.
Recovery time
Recuperation time can vary based on the patient’s age, overall health, and the technique performed. In general, patients should anticipate spending one to three days in the hospital and may need up to six weeks to recuperate.
Follow your doctor’s advice for physical activity, medications, and wound care during the recovery period to prevent complications and promote a smooth recovery.
Alternatives
Depending on the patient’s condition and wishes, there are options that could be explored in some circumstances. These alternatives include, among others:
- Medications
In some circumstances, hormone therapy or nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to treat the signs and symptoms of conditions like endometriosis and fibroids.
- Uterine Artery Embolization
A minimally invasive treatment called uterine artery embolization involves closing off the blood arteries that carry small particles to the uterus. This can lessen symptoms and decrease fibroids.
- Endometrial Ablation
Endometrial ablation is a procedure that involves destroying the lining of the uterus to reduce heavy bleeding.
- Hysteroscopic Myomectomy
Hysteroscopic myomectomy is a minimally invasive procedure that removes fibroids from the uterus using a thin, lighted tube inserted through the cervix.
Benefits of Hysterectomy Surgery
Hysterectomy surgery can offer various benefits for women, depending on their individual health conditions and goals. Some of the most common benefits of hysterectomy surgery include:
- Relief from pain and discomfort caused by conditions such as endometriosis, adenomyosis, fibroids, or pelvic inflammatory disease
- Improvement in quality of life and mental health, especially for women who suffer from heavy menstrual bleeding, urinary incontinence, or sexual dysfunction
- Prevention or treatment of gynecologic cancer, such as uterine, cervical, or ovarian cancer
- Elimination of the risk of unwanted pregnancy, as hysterectomy is a permanent form of birth control
While the benefits of hysterectomy surgery may seem appealing, it is important to note that each woman’s experience may differ and that hysterectomy is not always the best or only option. Alternative treatments, such as medication, hormone therapy, or less invasive surgeries, may be more suitable for some women.
Risks of Hysterectomy Surgery
Like any surgical procedure, hysterectomy surgery carries some risks and potential complications, which should be discussed with your healthcare provider before undergoing the surgery. Some of the most common risks of hysterectomy surgery include:
- Pain, bleeding, infection, or scarring at the surgical site
- Damage to nearby organs, such as the bladder, ureters, or intestines
- Blood clots, which can lead to serious conditions, such as stroke, pulmonary embolism, or deep vein thrombosis
- Menopausal symptoms, such as hot flashes, mood swings, or vaginal dryness, if the ovaries are removed
- Sexual or urinary problems, such as reduced libido, vaginal shortening, or urinary incontinence
To minimize the risks of hysterectomy surgery, it is important to choose a skilled and experienced surgeon, follow pre-operative and post-operative instructions carefully, and monitor any unusual symptoms or complications.
Conclusion
Conclusion: hysterectomy surgery can be a difficult and life-altering choice for women with a variety of gynecologic disorders. By learning the types, benefits, and dangers of hysterectomy surgery, women can make an informed decision on their health care. See a trained gynecologist or surgeon to discuss the risks and benefits of each type of hysterectomy surgery and to compare them to other possible treatment choices.
While the comparative article has some basic information regarding hysterectomy surgery, this complete guide goes into far greater depth. It gives extensive explanations of each form of hysterectomy operation, as well as the accompanying benefits and hazards. It also provides practical recommendations for minimizing the risks and consequences associated with hysterectomy surgery, such as selecting an experienced surgeon and carefully following pre-and post-operative instructions.
Overall, this article might be a helpful resource for women who are considering hysterectomy surgery or who have previously undergone it. It delivers clear and straightforward information in an easily digestible format to assist women in making educated decisions on their healthcare alternatives.
FAQs
- Is a hysterectomy a major surgery?
Yes, a hysterectomy is considered a major surgery and carries some risks and potential complications.
- Can I still have children after a hysterectomy?
With the use of assisted reproductive technologies, you may still be able to conceive if your ovaries are still viable. Yet, the removal of the uterus will render pregnancy impossible.
- How long does it take to recover from a partial hysterectomy?
It may take up to six weeks to fully recover, depending on the patient’s condition and the approach utilized during the treatment.
- What are the risks of a hysterectomy?
Potential risks include bleeding, infection, damage to surrounding organs, vaginal prolapse, and hormonal changes.
- Are there alternatives to hysterectomy?
Indeed, alternatives to partial hysterectomy may include medicines, uterine artery embolization, endometrial ablation and hysteroscopic myomectomy, depending on the patient’s condition and preferences. Before making a decision, it is essential to consider all possibilities with your healthcare professional.
- Is a partial hysterectomy the same as a total hysterectomy?
No, a partial hysterectomy only involves the removal of the uterus, while a total hysterectomy involves the removal of both the uterus and cervix.
- How long does the procedure take?
The duration of the process can vary based on the technique employed and the patient’s unique situation, but it typically lasts between one and three hours.
- Will I experience menopause after a partial hysterectomy?
Menopause will not occur immediately if the ovaries are left unharmed. Yet, hormonal changes may gradually lead to menopause over time.
- Will I have to stay in the hospital after the procedure?
Most patients will stay in the hospital for one to three days following the procedure.
- When can I return to work after a partial hysterectomy?
Depending on the individual’s unique situation and job needs, the duration of time off work will vary, but most patients can return to work in four to six weeks. Follow your healthcare provider’s advice for going back to work after having a discussion about this.