Why Prolapse occurs after a Hysterectomy and How to Avoid it
Did you know that one of the possible causes of pelvic organ prolapse is having undergone a hysterectomy?
Today we will see the relationship between having undergone a hysterectomy and being more likely to suffer a pelvic organ descent, which we call a prolapse.
When we talk about hysterectomy we talk about the total or partial removal of the uterus or also called matrix. The removal of the uterus can affect the rest of the organs found in the pelvis and the complex system of muscles, ligaments, and the fasciae that makes up the pelvic floor.
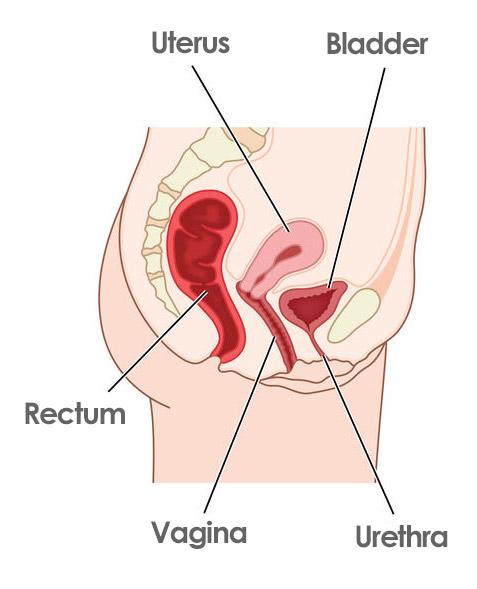
The uterus is one of the three organs that is integrated into the pelvic floor, we have the bladder in the anterior compartment, the uterus in the central or middle compartment, and in the back, we find the rectum. There is a complex system of interconnections between the organs, the muscles of the pelvic floor, the ligaments, the supporting tissues and this means that if we remove a central element such as the uterus, all these interconnection networks are affected.
And it is that a hysterectomy or removal of the uterus will cause what we call alterations in pelvic statics. In other words, those compartments that have not been operated on, the anterior compartment where the bladder is located or the posterior compartment where the rectum is located, may suffer alterations in their positions.
Before hysterectomy
So that you can better understand why pelvic statics is altered after a hysterectomy, observe how the relationship between the organs changes when the uterus is removed.
Under normal circumstances, we have the bladder, the uterus, and the rectum very close together, very connected in that space of the pelvis.
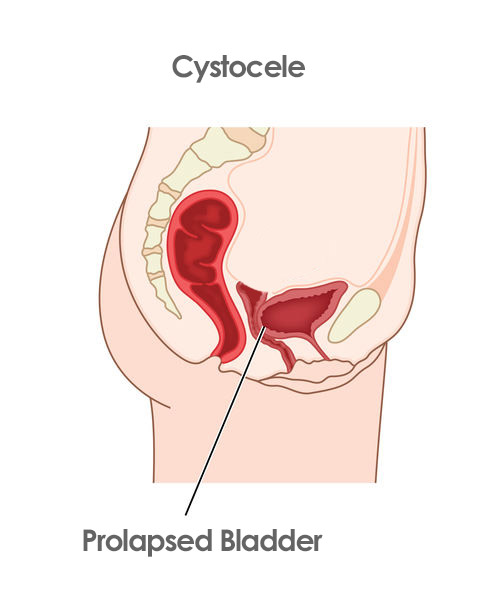
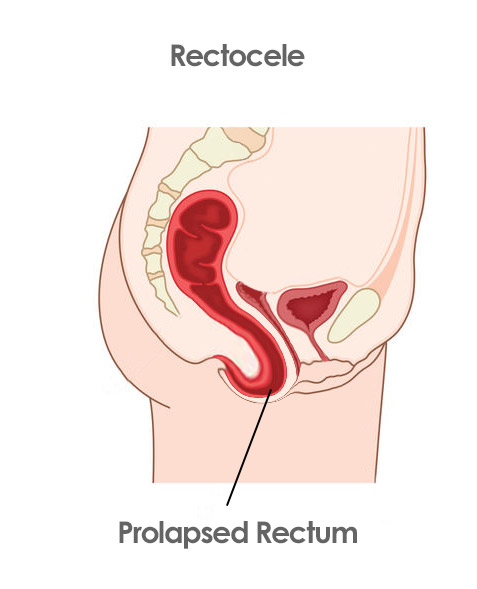
After hysterectomy
By eliminating this central element, both the bladder and the rectum will have an extra space in the center to move freely.

Bladder Prolapse
We now have a bladder that can go backward, which is what we call cystocele or bladder prolapse.
Rectal Prolapse
And we have the rectum that can come forward toward the area where the vagina is. Causing a rectocele. All this is caused by having eliminated that important central element that is the uterus.
How to prevent pelvic organ prolapse after hysterectomy
And now that you know the relationship between hysterectomy and the possibility of suffering pelvic organ prolapse, let’s see what you can do to prevent this from happening as much as possible.
Get the right information
First of all, I recommend you inform yourself how you are doing by reading this article. Now you know that there is a direct relationship between undergoing a hysterectomy and suffering from a prolapse. Many women who undergo this intervention are unaware of it, so share this article with those women who have undergone a hysterectomy or are going to undergo it. Because the information is very powerful and there are women who after years of a hysterectomy with the prolapse already present and one wonders how many cases could have been avoided simply by knowing this information in advance. So the first point you already have is the information.
Evaluate your Pelvic Floor
The second place is that you evaluate your pelvic floor and your abdomen with a physiotherapist, midwife, or gynecologist specialized in the pelvic floor. The surgeon who has carried out the surgical intervention does not have to know how your muscles are, how your abdomen manages the pressures, you will only see a pelvic floor specialist. It is important to know the state of the muscles that are going to support the rectum and the bladder that has been left with the modified space after the operation. Learn to perform recovery exercises and exercises so that intra-abdominal pressure does not affect your pelvic floor.
Know the Risk Factors
Tip number three is to know what the risk factors are, that is, the intra-abdominal pressures that endanger those organs, the bladder, the rectum, and that pelvic floor that at this time after a hysterectomy needs a lot of attention.
The factors are overweight and obesity, chronic cough, carrying weight, performing impact sports, or hyperpressive exercises such as classic abdominals. If you have had a hysterectomy and you are a constipated woman. We have to do something about it now, you already know that it is bad for the pelvic floor and to be able to suffer a prolapse second, you know that you are constipated third, we are going to get down to work to correct it and to prevent it from causing a prolapse. In this article, you have the explanation you need if this is your case.
Train your Abdomen and Pelvic
The fourth tip is to train your abdomen and your pelvic floor. Because as we have seen right now we are much more vulnerable to prolapse. Prolapse can be avoided by knowing the risk factors as I have just told you and by training the pelvic floor and the abdomen to compensate for those hyperpressures that it is sometimes inevitable to suffer or experience in everyday life. For example, if you have a young daughter or son and you have to lift them in your arms, the more trained your core and pelvic floor are, the better you are going to compensate, support, and cope with those pressures of everyday life.
We should also see the most appropriate type of exercise for each case with a pelvic floor specialist. In general, they use hypopressives, the 5p method, global training in which a lot of attention is paid to the core and the pelvic floor. Kegel exercises, not in all cases, but in some. Proprioception exercises and we can also help ourselves with tools such as biofeedback, electrostimulation, Kegel exercisers, etc. to obtain better results
Maintain regular check-ups
In fifth and last place. You must maintain your regular check-ups. Imagine that you have already done a pelvic floor rehabilitation, you are delighted, you feel much fitter, much more content with both your abdomen and your pelvic floor. You say goodbye to your physiotherapist and after years or months, you notice a loss of urine or feel heavy.
And this happens because, like any other muscle in our body, when we stop exercising it loses its tone, loses its strength, loses its well-being.
Therefore, we must undergo regular check-ups to see how is your pelvic floor, how your abdomen is. Maybe you have to adjust that exercise, routine that was recommended to you back in the day, and that now you may need some change. In this way, through periodic controls, we also reaffirm our commitment to take care of ourselves. It is a fact that we all forget from time to time, and we have to be sincere. If you don’t go to the physical therapist regularly it could be that the exercises end up in the last list of your priorities.
So once every three months, every 6 months, each person will see what is the appropriate frequency, it is recommended that you go to your physiotherapist to re-activate yourself and recommit to your intimate well-being.





