Understanding Vaginal Cancer After Hysterectomy: Causes, Symptoms, and Treatment Options
Introduction
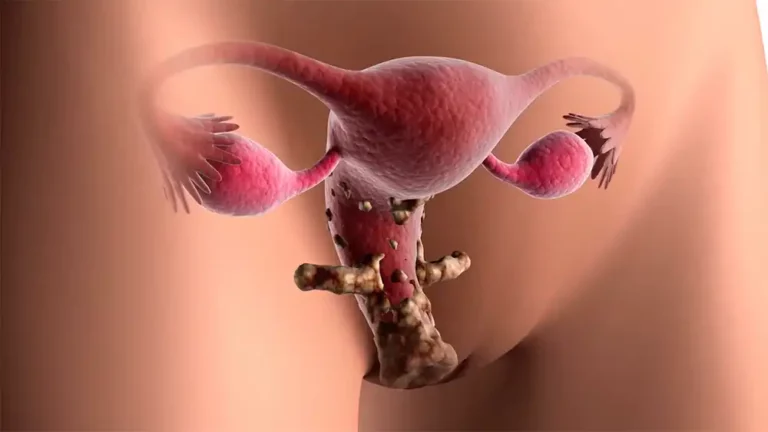
The uncommon disease known as vaginal cancer affects the muscular tract that connects the uterus to the external genitalia. It typically affects women over the age of 60, and exposure to diethylstilbestrol (DES) or the human papillomavirus (HPV infection) may be the cause. As a consequence of vaginal cancer, the vaginal area may bleed, leak, ache, or form a lump. Early detection increases the probability of a cure. Depending on the form and stage of the cancer, surgery, radiation therapy, or chemotherapy may be used to treat vaginal cancer.

Background Information
Overview of hysterectomy
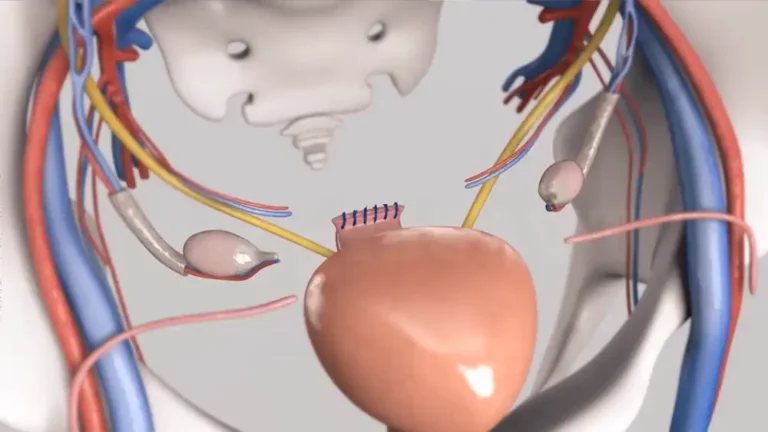
A hysterectomy is a procedure in which the uterus (womb) of a woman is removed. While pregnant, the fetus is fed by the uterus, a hollow muscular organ. The woman can no longer become pregnant or experience periods after having her uterus removed. In addition, the lady experiences menopause if her ovaries are also removed.
Types of hysterectomy
There are different kinds of hysterectomy depending on what part of the uterus is taken and how the surgery is done. These are the most common:
- Total hysterectomy is when the whole uterus, including the cervix, is taken out. This is the kind of abortion that most women have.
- Subtotal or partial hysterectomy: The cervix stays in place, and only the top part of the uterus is taken out. Even though it might not cause as many problems as a total surgery, it still needs to be checked for cervical cancer on a regular basis.
- In a Radical hysterectomy, the uterus, the cervix, the tissues around it, the ovaries, the fallopian tubes, the lymph nodes and part of the vagina are removed. It is the most invasive type of hysterectomy and is done when the cancer is very far along.
In addition, depending on the access route to perform the surgery, the following can be distinguished:
- Abdominal hysterectomy: A large incision is made in the abdomen and the uterus is removed through it.It is the most traditional way of performing a hysterectomy, but also the one that involves the most risk factors and complications.
- Vaginal hysterectomy: A cut is made at the top of the vagina and the uterus is removed through it. It leaves no visible scars and has a faster recovery than an abdominal hysterectomy.
- During a Laparoscopic hysterectomy, several tiny incisions are made in the abdomen, and a laparoscope with a camera is inserted. Using the laparoscope, the uterus is dissected and removed piece by piece. It is a minimally invasive hysterectomy that reduces pain, blood loss, and infection risk.
- Robotic hysterectomy: This is a variant of laparoscopic hysterectomy in which the surgeon controls the surgical instruments with increased precision and mobility using a robotic system.
Why is a hysterectomy done?
These are the most typical reasons for hysterectomy:
The benign tumors known as uterine fibroids can result in heavy monthly bleeding, pelvic pain, strain on other organs, and problems with fertility.
Endometriosis is a condition where the uterine lining grows outside of the uterus, causing pain, bleeding irregularities, or infertility.
Adenomyosis is a disorder that causes painful and heavy periods because the uterine lining tangles with the muscular uterine wall.
Due to decreased supporting muscles and ligaments, uterine prolapse is the descent of the uterus from its usual position toward the vagina. It may cause sexual distress, urine incontinence, and issues emptying the bladder or rectum.
People with early-stage cervical cancer and other gynecologic cancers are often treated with a hysterectomy since it is an effective method of disease management.
What is the relationship between hysterectomy and vaginal cancer?
The risk factors of developing posthysterectomy vaginal cancer may vary based on the specifics of the procedure and the patient’s medical history.
- Total Hysterectomy. Since most occurrences of vaginal cancer begin in the upper region of the vagina, a total hysterectomy, which eliminates the uterus and cervix, may lower the risk of this disease. Cancer can still grow in other areas of the vagina, so the risk is not entirely gone.
- Partial Hysterectomy. When the cervix is left in place during a hysterectomy, vaginal cancer risk is the same as with a full hysterectomy. In fact, it may raise your risk if it was performed to treat a condition caused by the human papillomavirus (HPV infection), such as cervical dysplasia or cancer. The human papillomavirus (HPV) can infect both the cervix and the vagina making it a potential cause of vaginal cancer.
- Hysterectomy for prenatal exposure to diethylstilbestrol (DES) may raise the risk of vaginal cancer. Between 1940 and 1971, DES, a synthetic hormone, was used to stop miscarriages. An uncommon form of cancer termed clear cell adenocarcinoma in the vagina or cervix is more likely to affect women who were exposed to DES when they were still growing. Although some of these women underwent hysterectomies to avoid or treat this malignancy, the danger is still present because cancer can recur in the vagina.
Some hysterectomy patients may experience a decreased risk of vaginal cancer after the procedure, but this risk is not totally eliminated. This is due to the fact that vaginal cancer can manifest itself anywhere in the vagina, including at the point where it joins the cervix at the bottom.
Therefore, after a hysterectomy, women should continue to get Pap tests and other vaginal cancer screening procedures like colposcopy. These tests can find aberrant cell alterations before they develop into cancer.
Vaginal Cancer Symptoms
Additionally, it’s crucial to keep an eye out for any potential vaginal cancer signs, such as:
- Abnormal vaginal bleeding, especially after menopause or after intercourse
- Watery or foul-smelling vaginal discharge
- Mass or lump in the vagina
- Pain when urinating or defecating
- Pelvic pain or during sexual intercourse
Any worrisome symptoms should be reported to a doctor as soon as possible in order to make an accurate diagnosis and obtain the best care.
Causes of Vaginal Cancer
Vaginal cancers are a rare type of cancer that originates in the vagina, the muscular tube that connects the uterus to the external genitalia. There are different types of vaginal cancer depending on the type of cell where cancer started, the most common being squamous cell carcinoma. Vaginal cancers can cause symptoms such as abnormal vaginal bleeding, watery discharge, painful urination or pelvic pain, but sometimes they don’t cause any signs until they are advanced.
What factors can increase the risk of developing vaginal cancer?
Even though no one knows for sure what causes vaginal cancer, there are some things that can make it more likely to happen, such as:
Surgical procedure
Some women who have had a hysterectomy (the uterus is removed) or severe trachelectomy (the cervix is removed) are more likely to get vaginal cancer. This is because these treatments can leave part of the cervix in the vagina and the cells of the cervix can turn cancerous over time.
Radiotherapy
Radiation therapy is a way to treat cancer by killing cancer cells with high-energy rays. But it can also hurt good cells and make it more likely that a second cancer will grow in the area where the first one was. Women who have had pelvic radiation treatment for cancers like cervical cancer or endometrial cancer have a higher chance of getting vaginal cancer.
Genetic factors
Some women are more likely to get vaginal cancer because of their genes. For example, women with Lynch syndrome, an inherited condition that raises the chance of several types of cancer, are more likely to get vaginal cancer than women without the condition. Other rare genetic conditions, like Peutz-Jeghers syndrome or Li-Fraumeni syndrome, have also been linked to vaginal cancer.
Human papillomavirus (HPV)
The common virus HPV can infect the skin and mucous membranes of the genitals and is spread through sexual contact. Only a few of the more than 100 different kinds of HPV are regarded as high risk because they can result in precancerous (vaginal intraepithelial neoplasia ) or cancerous cell alterations. The main cause of vaginal cancer (and cervical cancers), particularly squamous cell carcinoma, is HPV. About 70% of cases of vaginal cancer are thought to be HPV infection related.
Other risk factors
In addition to the factors mentioned above, there are other factors that can increase the risk of developing vaginal cancer, such as the following:
- Having been exposed to diethylstilbestrol (DES) before birth. DES is a synthetic hormone that was used between 1940 and 1971 to prevent miscarriage and pregnancy complications. However, the daughters of the women who took DES were found to have a higher risk of developing a rare type of vaginal cancer called clear adenocarcinoma.
- Having a personal or family history of other types of gynecologic cancer, such as cervical cancer, cervical intraepithelial neoplasia, ovarian cancer or endometrial cancer.
- Having a weakened immune system from diseases such as HIV/AIDS or from drugs that suppress it, such as those used to prevent rejection of transplanted organs.
- Cigarette smoking, which can damage the DNA of cells and make it easier for HPV infection.
- Having multiple sexual partners or starting sexual intercourse at a young age, which increases exposure to HPV and other sexually transmitted infections.
- Having poor intimate hygiene or using irritating products in the genital area, which can cause inflammation and upset the natural balance of vaginal flora can be another risk factor.
How can vaginal cancer be prevented?
Although there is no surefire way to avoid vaginal cancer, there are activities that can be taken to lower the risk, including the ones listed below:
- Get an HPV vaccine. The most prevalent and dangerous strains of HPV that cause cancer are covered by vaccinations. It is advised to immunize boys and girls between the ages of 11 and 12, but individuals older than 26 can also receive the vaccine. It is crucial to acquire the vaccine before having sex since it is ineffective if you have already been exposed to HPV.
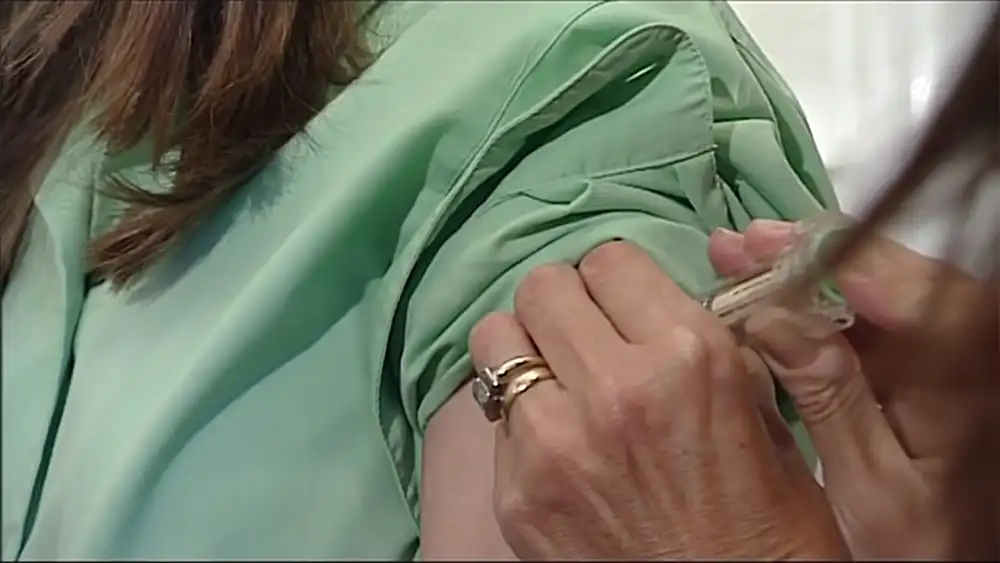
- Get tested for HPV cervical cancer screening. These tests can detect the presence of HPV or abnormal cells in the cervix that can become cancer. If an HPV infection or precancerous lesion is detected, it can be treated before it progresses to cancer.

- Avoid exposure to DES. The use of DES has been banned since 1971, but if you are a woman who was exposed to DES before birth, you should tell your doctor and get screened more often.
- Using condoms when having sexual contact. Condoms can make it less likely that you will get HPV or other sexually transmitted diseases that can lead to vaginal cancer. But condoms don’t fully protect against HPV because HPV can get into places that condoms don’t cover.
- Limit the amount of sexual partners you have and choose people who have had few or no sexual partners before you. This makes it less likely that you will get HPV or other sexually transmitted diseases.
- Quit smoking or not start smoking. Several types of cancer, including vaginal cancer, are more likely to happen if you smoke.
- Keep good personal hygiene and stay away from items that irritate. The genital area should be washed with water and light soap, dried well, and cotton underwear should be worn. When it comes to the genital area, you shouldn’t use vaginal douches, personal deodorants, powders, or perfumes because they can cause irritation and infections.
Diagnosis of Vaginal Cancer
Your doctor may do the following tests to find out if you have vaginal cancer:
Physical exam
The doctor can look at the outside of the genitalia and feel the belly for any lumps or abnormalities.
Pelvic exam
In order to feel the uterus and ovaries, the doctor may press on the abdomen with one hand while inserting two fingers into the vagina. A speculum can be used to open the vaginal opening and shine a light on the cervix and vagina. Your doctor may do a Pap smear during a pelvic exam, which entails collecting a sample of cells from your cervix using a brush or spatula and sending them to a lab for analysis. A Pap smear is typically used to detect cervix cancer, but it can also occasionally detect cancerous cells in the fetus.
Biopsy
A biopsy is the only test that can confirm the diagnosis of vaginal cancer. It consists of removing a sample of suspicious tissue from the vagina with forceps or a needle and sending it to a laboratory for analysis. The vaginal biopsy may be done during a colposcopy, which is an examination of the vagina with a special instrument that has a light and a magnifying glass , called a colposcope. Colposcopy allows the doctor to see the surface of the vagina in more detail and detect any areas of abnormal cells.
Imaging tests
Imaging tests are examinations that use X-rays, sound waves, magnetic fields or radioactive substances to produce images of the body’s interior. The doctor can use imaging tests to determine whether the cancer has migrated to surrounding organs or surrounding tissue. The following imaging tests can be utilized to diagnose vaginal cancer:
- Using X-rays, radiography obtains images of the bones and internal organs.
- A computed tomography (CT) scan utilizes a machine that rotates around the patient’s body and captures a series of images from various angles. These images are combined to produce a three-dimensional image of the body that is rich in detail.
- Magnetic resonance imaging (MRI): Using an enormous magnet, radio waves and a computer, magnetic resonance imaging (MRI) creates detailed images of the body.
- PET scan: utilizes a radioactive chemical known as a tracer which is injected into a vein and collected in locations where there is abnormal cell activity. A specialized camera detects the tracer’s radiation and generates an image depicting the location of cancer cells in the body.
Staging of Vaginal Cancer
Stages of vaginal cancer indicate the extent or spread of cancer from its origin in the vagina to other parts of the body. Knowing the stage of cancer helps determine the prognosis and the most appropriate treatment for each case.
How are the stages of vaginal cancer determined?
The International Federation of Gynecology and Obstetrics (FIGO) method and the American Joint Committee on Cancer (AJCC) TNM (Tumor, Node, Metastasis) system are both used to categorize the progression of vaginal cancer. There are three primary components shared by both systems:
- The location and size of the tumor (T) in the vagina and surrounding tissues.
- Lymph nodes (N) are part of the immune system and serve as filters that can catch cancer cells as they pass through the blood or lymph.
- Cancer that has spread to other organs, including the lungs or liver, is said to have metastasized (M).
The sum of these indicators is used to designate an overall stage, with stage 0 being the earliest stage and stage IV the most advanced. A physical examination, biopsy, and imaging tests can all be used to establish the stage either before or after surgery.
What are the stages of vaginal cancer?
Described below are the phases of vaginal cancer:
- Stage 0: This precancerous condition is also known as carcinoma in situ or vaginal intraepithelial neoplasia (VAIN) and is characterized by the presence of aberrant cells on the surface of the vagina that have not yet invaded deeper layers. It typically causes no symptoms and can be treated surgically or with local therapy.
- Stage I: The cancer is contained to the vaginal wall and has not metastasized to lymph nodes or surrounding tissues. It has two substages: IA for tumors that are less than 2 cm in diameter and IB for tumors that are more than 2 cm. Chemotherapy, surgery or radiation therapy are all possible forms of treatment.
- Stage II: Lymph nodes and distant organs are unaffected, but cancer has progressed to tissues close to the vagina, such as the uterus, bladder or rectum. Chemotherapy or radiation therapy may be used in conjunction with surgery as a form of treatment.
- Stage III: Cancer has spread to pelvic or groin lymph nodes, but not to distant organs. It is divided into two substages: IIIA, if the cancer only affects the pelvic lymph nodes; and IIIB, if the cancer affects the inguinal lymph nodes. Treatment may include surgery combined with radiation therapy or chemotherapy.
- Stage IV: Cancer has spread to distant organs or invaded vital structures such as the pelvic wall or bone. It is divided into two substages: IVA, if the cancer affects nearby organs such as the bladder, rectum, or bone; and IVB, if the cancer affects distant organs such as the lungs, liver, or brain. Treatment may include radiation therapy or chemotherapy
Vaginal Cancer Treatment Options
Treatment of vaginal precancers
Precancers of the vagina are alterations in the cells of the vagina that, if left untreated, can progress into cancer. They are referred to as vaginal intraepithelial neoplasia (VAIN) and are categorized as low-grade or high-grade according to the degree of cell abnormality.
Precancers of the vagina can be detected with a pelvic exam, Pap smear, or colposcopy, an exam that employs a lighted instrument and a magnifying lens to examine the vaginal surface in greater detail. If a suspicious area is detected, a biopsy can be conducted, which involves the removal of a tissue sample for laboratory analysis.
Treatments for vaginal precancers include:
- Laser surgery: A laser beam is used to destroy abnormal cells.
- Topical therapy: A cream or gel is applied with drugs that kill abnormal cells or stimulate the immune system to fight them.
Many cases of low-grade VAIN (vaginal intraepithelial neoplasia) go away on their own, so some doctors prefer to watch it without starting treatment. If the VAIN area does not go away or worsens, treatment can be started. High-grade VAIN is more likely to progress to cancer, so it is usually treated right away.
Treatment of invasive vaginal cancer
Invasive vaginal cancer is cancer that has grown beyond the superficial layer of the vagina and can affect other nearby organs or spread to other parts of the body. Treatment of invasive vaginal cancer usually includes radiation therapy and surgery, and in some cases also chemotherapy, targeted therapy, or clinical trials.
Radiotherapy
Radiation therapy is the use of x-rays or other high-energy particles to kill cancer cells. It can be given from an external source (external radiation therapy) or from an internal source (brachytherapy), which involves placing radioactive material inside or near the tumor.
Radiation therapy may be used as the primary treatment for vaginal cancer in its early stages or as a supplement to surgery to reduce the risk of recurrence. It can also be used to treat advanced vaginal cancer symptoms.
Radiation therapy can cause adverse effects such as irritation of the skin, fatigue, nausea, diarrhea, vaginal dryness, vaginal bleeding and urinary issues.
Surgery
Surgery is the use of surgical instruments to remove the tumor and surrounding healthy tissue. The types of surgery that can be used to treat vaginal cancer are :
- Local excision: The tumor and a small amount of healthy tissue around it are removed. It can be done with a scalpel, a laser or an electric loop.
- Vaginectomy: Part or all of the vagina is removed. The vagina can be reconstructed with tissue from another part of the body.
- Hysterectomy: The uterus and cervix are removed. It can be done abdominally, vaginally, or laparoscopically. If the cancer has spread to the pelvic lymph nodes, they may also be removed in the same operation (lymphadenectomy).
Surgery can cause side effects such as pain, bleeding, infection, urinary or sexual problems, or swelling in the legs.
Chemotherapy
Chemotherapy is a way to kill cancer cells by using drugs. It can be taken by mouth or put into a vein.
Chemotherapy can be used with radiation treatment to make it work better (chemoradiation) or to treat cancer that has spread to other parts of the body.
Chemotherapy can make you sick, make you throw up, cause hair loss, make you tired, give you infections or hurt your organs.
Targeted Therapy
Targeted therapy is the use of medications that specifically target cancer cells without harming healthy cells. It can be used to treat vaginal cancer varieties with specific genetic or molecular mutations. Some vaginal malignancies, for instance, produce the protein epidermal growth factor receptor (EGFR), which promotes their growth and survival. Targeted therapy can inhibit this protein and delay the progression of cancer.
Orally or intravenously, targeted therapy can be administered. Targeted therapy can result in adverse effects such as rash, diarrhea, elevated blood pressure, and liver issues.