PCOS Treatment Options: Is Hysterectomy the Right Choice?
Understanding Polycystic Ovary Syndrome
What is Polycystic Ovarian Syndrome (PCOS)
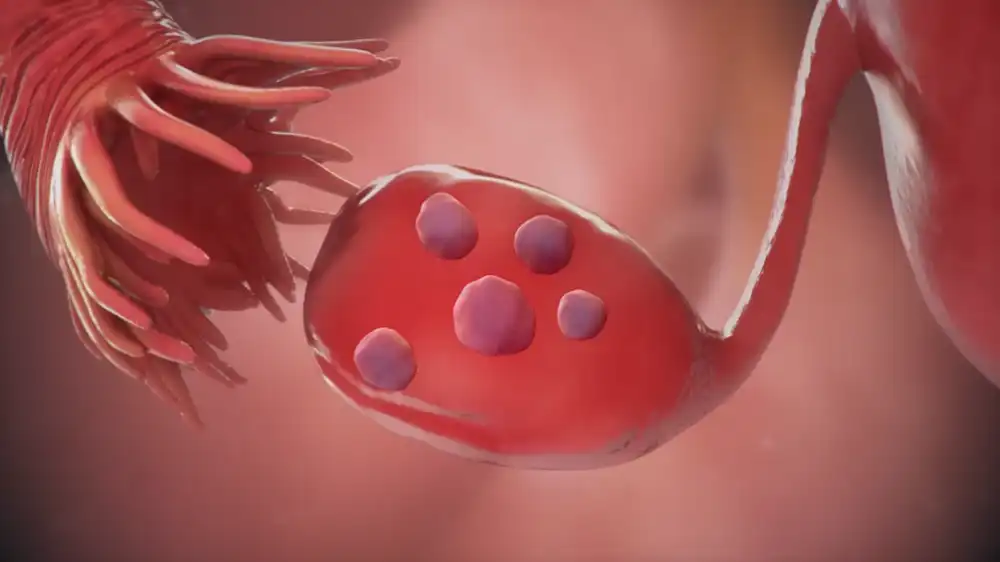
PCOS is a hormonal disorder that impacts between 5 and 10 percent of women of reproductive age1. It is characterized by the presence of ovarian fibroids, elevated androgen (male hormone) levels, and alterations in ovulation and menstruation2. Infertility, obesity, insulin resistance, diabetes, cardiovascular disease, melancholy, and endometrial cancer can all be caused by PCOS.
Symptoms and diagnosis of Polycystic Ovary Syndrome
Polycystic Ovary Syndrome PCOS is a hormonal disorder characterized by a variety of symptoms, the intensity and frequency of which can differ from woman to woman. The most PCOS symptoms are:
• Inconsistent or absent menstrual cycles (irregular periods), which can impede ovulation and fertility.
• Hirsutism, characterized by excess hair growth (on the face and body), is caused by an increase in androgen (male sex hormones) levels.
• Acne can be intense and resistant to conventional treatments.
• Androgenic alopecia is a prevalent pattern of male hair loss.
• Obesity and weight gain, particularly in the abdomen, can increase the risk of high insulin levels and diabetes.
• Polycystic ovaries are enlarged ovaries with multiple cysts or follicles that are incapable of producing mature eggs.
Polycystic Ovary Syndrome is diagnosed by the presence of at least two of these symptoms and the exclusion of other possible causes. To achieve this the physician may conduct a series of tests, including:
• Exam of the pelvis to detect abnormalities or growths in the reproductive organs.
• Blood tests to determine the concentrations of hormones such as testosterone, prolactin, thyroid-stimulating hormone and adrenal hormones. Fasting cholesterol, triglycerides and glucose are also quantifiable.
• Ultrasound, to assess the appearance of the ovaries and the thickness of the endometrium (uterine lining).
Impact of PCOS on fertility and overall health
PCOS is one of the most frequent causes of female infertility since it alters ovulation and makes conception difficult. However, many women with PCOS can achieve a pregnancy with proper treatment, which may include medications to stimulate ovulation or assisted reproductive techniques.
PCOS can also affect the general health of women who suffer from it, increasing the risk of developing various complications in the short and long term.
Some of these complications are:
• Metabolic syndrome, which is a set of factors that increase the risk of cardiovascular disease and diabetes. These factors are: abdominal obesity, arterial hypertension, dyslipidemia (high cholesterol and triglycerides) and hyperglycemia (high glucose).
• Type 2 diabetes, which occurs when the body does not produce or properly use insulin. High insulin levels is a feature of PCOS that predisposes to diabetes.
• Endometrial cancer, which originates in the tissue that recovers from the uterus. The risk of this cancer is increased by the lack of ovulation and regular menstruation, which causes prolonged exposure of the endometrium to estrogens without counteracting them with progesterone.
• Depression and anxiety, which may be a consequence of the psychological and emotional impact of PCOS. The physical symptoms of PCOS (like hair growth) can affect women’s self-esteem, female identity, and sexuality. Additionally, chronic stress and inflammation can upset the neurochemical balance of the brain.
What is a hysterectomy?
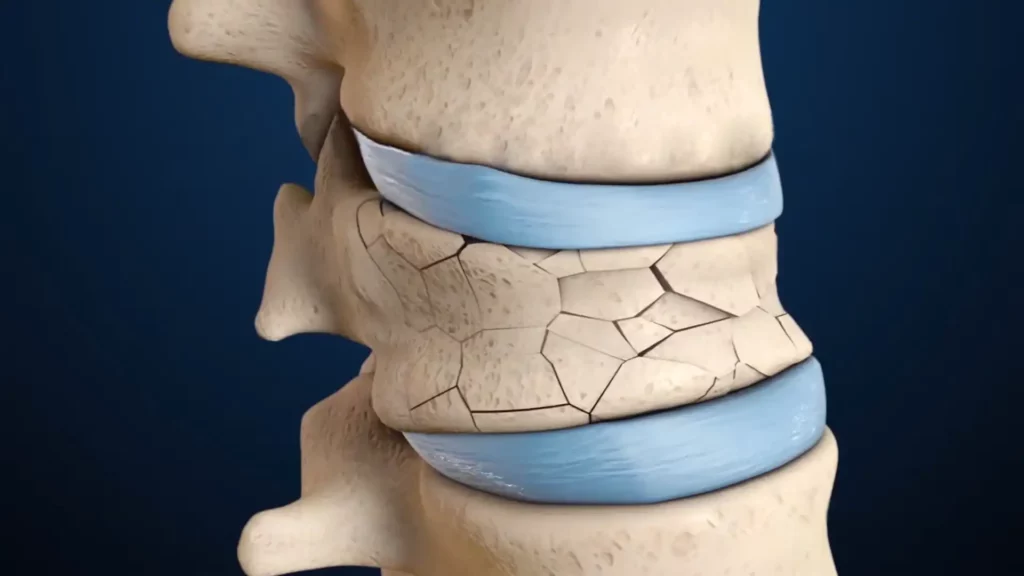
In a hysterectomy, the uterus and, occasionally, the ovaries and fallopian tubes are also removed. It may be performed due to abnormal uterine bleeding, fibroids, endometriosis, prolapse, or cancer, among other conditions. Women who undergo hysterectomy experience both physical and psychological side effects, including loss of fertility, early menopause, hormonal abnormalities and an increased risk of osteoporosis.
Based on the scope and technique of the operation, there are various types of hysterectomy:
• A subtotal or partial hysterectomy just removes the uterine corpus; the cervix is left in place. It is the least intrusive and recovers the fastest.
• Removal of the uterus and cervix during a total hysterectomy. It is the most popular and advised way to avoid cervical cancer.
• During a radical hysterectomy, the uterus, cervix, upper vaginal wall, and surrounding tissues are removed. Because of how aggressive it is, it is only used in cases of advanced cancer.
In addition, depending on the access route to the uterus, the following types of surgery can be distinguished:
• Abdominal hysterectomy: A cut is made in the abdomen similar to a cesarean section. It allows better visualization of the area, but has a higher risk of complications and a slower recovery.
• Vaginal hysterectomy: A cut is made in the vagina. You have less risk of infection and bleeding, and a faster recovery. However, it is not suitable for all cases.
• Laparoscopic hysterectomy: Small cuts are made in the belly button or vagina through which surgical instruments and a camera are inserted. It is less invasive and has a faster recovery. It requires more skill from the surgeon and can have specific complications.
• Robotic hysterectomy: It is similar to laparoscopic, but with machines that perform the procedure. It has the same advantages and disadvantages as the laparoscopic one.
Is a hysterectomy a cure for PCOS?
Some women with PCOS may consider a hysterectomy as an option to relieve their symptoms or prevent long-term complications. However, hysterectomy is not a cure for PCOS, but an extreme measure that is only recommended in very specific cases and under medical criteria.
Here are some reasons why hysterectomy can’t cure PCOS:
Polycystic Ovary Syndrome PCOS is a hormonal disorder that affects not only the uterus but the entire body. The ovaries will continue to produce androgens and cause hormonal imbalance with symptoms such as hirsutism (excess hair), acne, and alopecia even if the uterus is removed.

When the ovaries and uterus are removed together, a surgical menopause occurs, accompanied by a precipitous decline in estrogen and progesterone levels. This can result in other symptoms like hot flashes, vaginal dryness, libido loss, urinary incontinence, mood fluctuations, and osteoporosis. Additionally, estrogens protect against heart disease, which is more prevalent in women with PCOS.
Hysterectomy does not eliminate the risk of developing diabetes or insulin resistance, which are key factors in PCOS. In fact, surgical menopause can increase insulin resistance and worsen glycemic control.
Hysterectomy has a psychological and emotional impact on women who undergo it. It can affect your self-esteem, your feminine identity and your sexuality. It can also generate feelings of loss, grief or depression for not being able to have biological children.
Hysterectomy may be an option for PCOS in the following instances:
Gynecologic cancer: If you have cancer of the uterus, cervix, or ovary, you may need a hysterectomy to remove the tumor and prevent it from spreading. A partial, total, or radical hysterectomy can be chosen depending on the type and stage of cancer and it can be combined with radiotherapy or chemotherapy.
Abnormal uterine bleeding: If you have excessive or irregular uterine bleeding caused by hormonal imbalances or uterine fibroids and it doesn’t respond to medical or conservative treatments, a hysterectomy may be a permanent solution. In addition, the risk of anemia or endometrial cancer associated with chronic bleeding can be prevented.
Pelvic pain: If you have severe or disabling pelvic pain caused by endometriosis or uterine prolapse and it doesn’t respond to medical or conservative treatments, a hysterectomy may be an option to improve your quality of life. However, pelvic pain may have other causes that are not resolved by hysterectomy.
What alternatives are there to hysterectomy to treat PCOS?
PCOS treatment must be individualized and adapted to the needs and objectives of each woman. There is no definitive cure for PCOS, but there are treatment options that can help control symptoms and prevent long-term complications.
Some of these options are:
Lifestyle changes: A healthy diet, low in sugar and fat and regular physical exercise can help you lose weight, improve insulin sensitivity, regulate ovulation and reduce cardiovascular risk. It is also recommended to avoid tobacco and alcohol.
Hormonal contraceptives: Birth control pills, patches, injections, vaginal rings, or intrauterine devices that contain estrogens and progestins can regulate the menstrual cycle, decrease abnormal uterine bleeding, control hirsutism and acne and prevent endometrial cancer. However, they can have side effects such as weight gain, thrombosis, or depression.

Antiandrogens: These drugs block the action of androgens and may improve hirsutism and acne. The most commonly used are spironolactone, flutamide and finasteride. They should be combined with hormonal contraceptives to avoid unwanted pregnancies, since they can cause fetal malformations.
Insulin Sensitizers: These drugs increase glucose uptake by cells and decrease insulin production by the pancreas. The most widely used is metformin, which can help you lose weight, regulate ovulation and improve cholesterol levels. It can also reduce the risk of diabetes and cardiovascular disease.
Fertility drugs: These drugs stimulate ovulation and increase the chances of pregnancy in women with PCOS who want to conceive. The most widely used is clomiphene citrate, which is taken orally for 5 days at the beginning of the menstrual cycle. Other medications include gonadotropins, which are injected subcutaneously or intramuscularly and letrozole, which is taken orally.
Surgery: Laparoscopic ovarian surgery, also known as ovarian drilling, involves making tiny incisions in the ovaries to increase ovulation and decrease testosterone production. It is only used in situations where reproductive medications have failed or are inappropriate to use.
Conclusion
Complex disorder polycystic ovarian syndrome necessitates a thorough and individualized treatment plan. Only extremely rare circumstances should hysterectomy be considered because it is not a treatment for PCOS. Other therapy options exist that can enhance the quality of life for PCOS-afflicted women and shield them from its side effects.