Tackling Cervical Dysplasia: The Role of LEEP and Hysterectomy
The basics of cervical dysplasia and LEEP
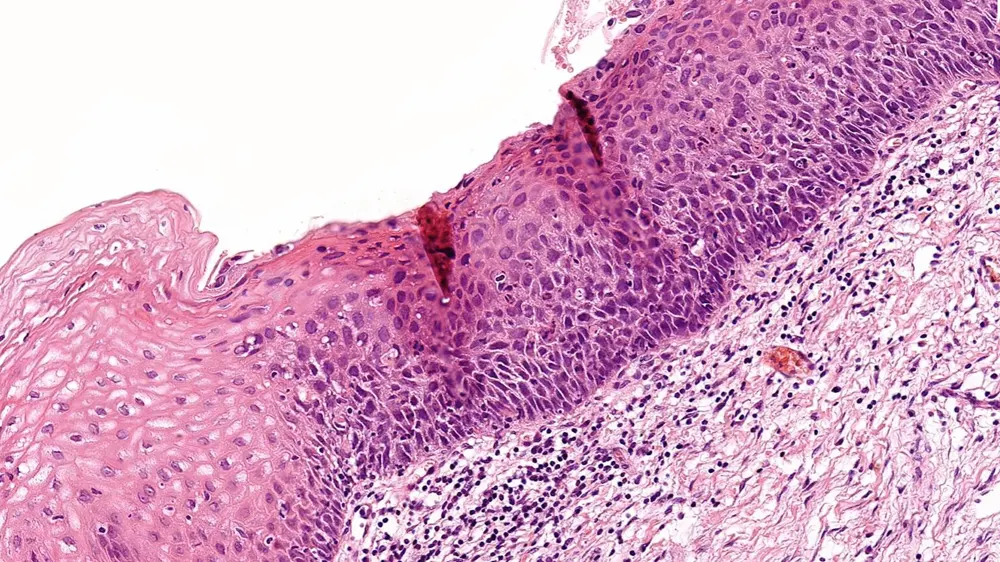
Cervical Dysplasia
Understanding the principles will help allay some of your worries about cervical dysplasia, which can be a terrifying and baffling diagnosis. In essence, cervical dysplasia also know as Cervical Intraepithelial Neoplasia (CIN) is a change in the cervix’s cells (becoming abnormal cells), which are located in the lowest part of the uterus and link to the vagina. If neglected, this condition could lead to cancer.
So what is the reason for cervical dysplasia? Well, there are a few risk factors, such as smoking, immune system deterioration, and specific HPV infection. The sexually transmitted human papillomavirus, also known as HPV, can result in genital warts and, in some circumstances, cancer. This is why routine Pap tests and Cervical Screening (HPV testing) are so important. Early abnormalities can be found with Pap smears, allowing for treatment before any disease progression.

What is LEEP?
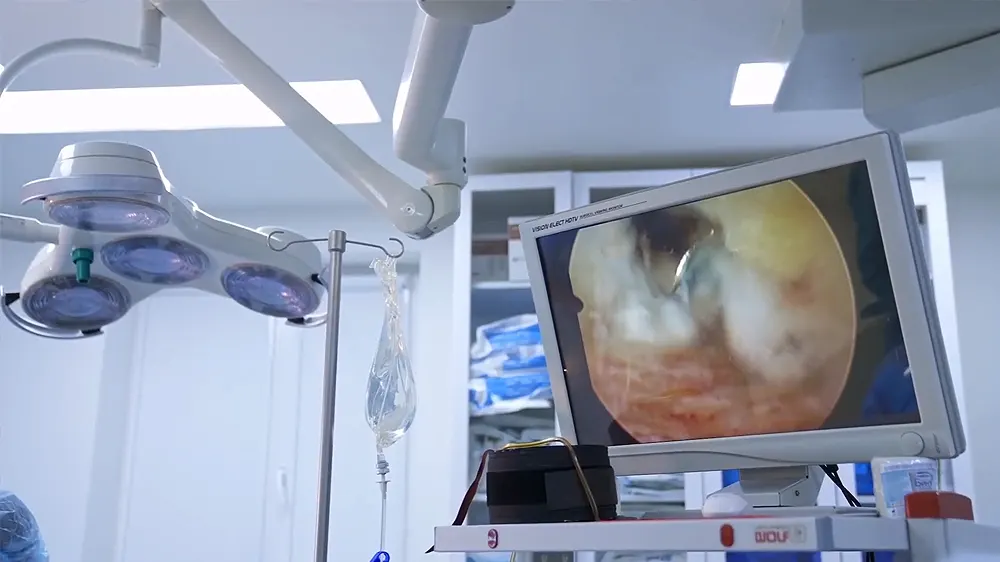
The surgical method known as LEEP, or loop electrosurgical excision procedure, is used to remove abnormal cells. This technique uses a small wire loop that is heated with an electrical current and is often carried out in a doctor’s office or clinic.
After the procedure, the removed abnormal tissue (abnormal cervical cells) is sent to a laboratory for examination. This is an important step in accurately diagnosing the condition and determining if further treatment is needed. In some cases LEEP may be used to remove tissue for diagnostic purposes , such as in cases of cervical cancer.
LEEP is advantageous because it is a minimally invasive procedure that can be performed swiftly and with minimal discomfort. The procedure typically takes less than thirty minutes, and the majority of women can resume normal activities the same day. LEEP is also a highly effective treatment for cervical abnormal cells, with an over 90% success rate.
After the loop electrosurgical excision procedure, you may have some vaginal bleeding or discharge for a few weeks. This is normal and is due to scarring of the cervix. You should avoid having sex, using tampons, or douching until your doctor tells you it’s okay. You should also avoid heavy exercise or heavy lifting for a few weeks.
It has few complications and does not affect your fertility or your ability to have vaginal deliveries in the future. However, you should continue to have a regular cervical screening (Pap smear test) to detect any changes in the cervix.
How Many LEEP Procedures Before Hysterectomy?
The decision to do one or more Loop Electrosurgical Excision Procedures or a hysterectomy depends on each case and the opinion of your doctor. The type and grade of abnormal cells, the size and location of the tumor, the desire to have children in the future, and other factors must be taken into account.
The significance of LEEP in managing CIN
LEEP is essential for the treatment of Cervical Intraepithelial Neoplasia by removing abnormal cells before they can develop into malignancy. Typically performed on an outpatient basis, this procedure is fast and painless. In addition, Loop Electrosurgical Excision Procedure has a high success rate, with the majority of patients reporting no return of abnormal cervical cells.
Nevertheless, LEEP is not only a safe alternative for women with moderate to severe cervical dysplasia, but it is also effective. Even though every medical procedure entails some degree of risk, LEEP is typically regarded as low-risk, with few significant adverse outcomes recorded. In addition, LEEP permits a more precise examination of the excised tissue, which can assist medical professionals in determining the severity of the abnormality and informing their decisions regarding subsequent treatment.
The connection between LEEP and hysterectomy
The surgical removal of the uterus, or hysterectomy, may worry some women who are considering LEEP. Despite the fact that LEEP does not directly induce hysterectomy, it is nevertheless possible that a woman undergoing LEEP or other therapies for CIN will eventually need a hysterectomy.
Because Cervical Intraepithelial Neoplasia can develop into cancer if left untreated, this is the case. If cervical dysplasia is not identified and properly treated, this number could be considerably higher. LEEP becomes relevant in this situation. The Electrosurgical Excision Procedure LEEP, involves to remove abnormal tissue using a small wire loop. Following that, the tissue is taken to a lab for examination to look for malignant or precancerous abnormal cells.
LEEP is frequently used to treat cervical dysplasia because it is a simple, fast procedure that can be performed in the doctor’s office. However, LEEP may sometimes be combined with hysterectomy, the surgical removal of the uterus. This may be performed if the patient has other medical conditions that necessitate uterine excision, or if the Cervical Intraepithelial Neoplasia is severe and has not responded to previous treatments.
A hysterectomy is a significant operation that carries risks; therefore , it should only be considered after careful consideration and consultation with a physician. Sometimes, alternative therapies may be able to effectively treat cervical dysplasia without the need for a hysterectomy. LEEP or hysterectomy should be selected in conjunction with a healthcare professional based on the patient’s unique circumstances.
LEEP and hysterectomy: how long do you have to wait to reduce the risk of infections?
A recent study of nearly 1,200 women who had lesions or cervical cancer and who Loop Electrosurgical Excision Procedure to remove abnormal cells concluded the following:
After LEEP, some women needed a hysterectomy to completely remove the uterus.
It was found that the more time between LEEP and hysterectomy, the lower the risk of infections after hysterectomy.
The type of hysterectomy that was done influenced the risk of having infections after the hysterectomy.
Laparoscopic hysterectomy, which is a less invasive surgery done through small incisions in the abdomen, required more time between LEEP and hysterectomy to reduce the risk of infection than open abdominal or vaginal hysterectomy, which are larger surgeries made with an incision in the vagina or abdomen.
In order to account for additional variables like the stage of the cervical cancer, the length of the procedure and the anticipated blood loss, a statistical technique called logistic regression was employed to quantify the impact of time and kind of surgery on infectious morbidity.
When there was longer time between LEEP and hysterectomy and when the procedure was performed laparoscopically, the risk of infections was shown to be reduced. The study also discovered a relationship between time and surgery type, indicating that the type of surgery affected how time affected recovery.
When is LEEP Needed?
The severity of cervical dysplasia that requires LEEP
Cervical Intraepithelial Neoplasia is a condition where the cells of the cervix start to change to abnormal cells or precancerous cells. These changes can range from mild abnormalities to more severe changes. When it comes to treatment, the severity of the dysplasia determines the next steps.
Mild dysplasia is typically monitored and may not require any intervention. However, moderate to severe dysplasia may require more aggressive treatment. One such treatment is a loop electrosurgical excision procedure (LEEP).
Factors that determine if LEEP is the best course of treatment
The location of the dysplasia should also be taken into account because LEEP may not be appropriate for lesions that extend past the cervix.
Other risk factors include your age and general health. All surgical procedures have risks, even though LEEP is normally a risk-free technique. For those who are older or have underlying medical conditions, LEEP might not be a good option. It’s critical to discuss all options with your healthcare expert in order to choose the best course of action for your specific situation.
Finally, if future fertility is a concern, LEEP may not be the best option. While LEEP is a minimally invasive procedure, it does involve removing a portion of the cervix. This can increase the risk of preterm labor or other complications during pregnancy. Patients who wish to have children in the future may be better suited for other treatments that preserve the cervix, such as a cone biopsy or cold knife conization.
When do you need a hysterectomy if you have cervical cancer or lessions?
Before doing a hysterectomy other tests and treatments must be done to find out what type of lesion or cancer you have and how it can be cured. Some things you should know are:
Hysterectomy is not a treatment for the human papillomavirus (HPV infection), which is the cause abnormal cervical cells and cervical cancer. Even if you remove your uterus, you can still have the virus and develop abnormal cells, lesions or cancer in the vagina or vulva. For this reason, you should have every once in a while a HPV testing.

Hysterectomy is not suitable for low-grade lesions (low grade cervical intraepithelial neoplasia), which have very little risk of developing into cancer. In these cases, the risks and costs of hysterectomy are not justified. There are other simpler and safer treatments for these injuries.
Hysterectomy may be an option for high grade cervical lesions (high grade cervical intraepithelial neoplasia 2 or 3) or invasive cancer, which are more at risk of progressing and causing serious problems. But before doing a hysterectomy, a biopsy must be done with a procedure called LEEP or cone, which removes a part of the cervix for examination. This is to confirm the diagnosis and see if there is hidden cancer that was not found by other tests.
Hysterectomy can be of different types depending on how the uterus is removed: laparoscopically, vaginally, or through the open abdomen. Each type has its advantages and disadvantages, and may affect the risk of infection after surgery. The time that elapses between the LEEP or cone and the hysterectomy must also be taken into account, because it can influence healing and inflammation.
Hysterectomy can be a safe and effective surgery to treat cervical lesions or cancer (or prevent cervical cancer), but it must be done carefully and judiciously. Not all women need or benefit from a hysterectomy. Each case must be assessed individually and the best option offered for each woman.
Complications of Multiple LEEP Procedures
While LEEP procedures are generally safe, there are risk factors associated with them, especially if you’ve had multiple procedures.
Cervical incompetence is one of the main risks associated with multiple LEEP procedures. The cervix is weakened at this point which may result in early delivery or even a miscarriage. This is because the cervix may become weaker and less able to support a developing fetus as a result of the LEEP procedure, which removes a portion of it. Women who intend to have children in the future should be particularly concerned about this risk.
Cervical stenosis is a risk related to multiple LEEP procedures. When the cervix narrows, it can interfere with menstruation and even make it difficult to conceive. Women who have undergone multiple LEEP procedures may also be more susceptible to infection. It’s crucial to keep in mind that even though these risks are conceivable, they are still relatively infrequent. The advantages of having a LEEP procedure typically outweigh the risks, particularly if abnormal cells are not treated. However, it’s crucial to go over your risks with your doctor if you’ve had several LEEP procedures.
Your doctor might advise keeping an eye on your cervix while you’re expecting or taking into account a cerclage, a procedure that can support the cervix. In addition, if you have menstrual issues or difficulty conceiving, your doctor may recommend further testing or treatment. Additionally, minimizing your risk of infection is essential. This includes adhering to your physician’s postoperative care instructions and refraining from sexual activity for a time. In addition, you should be on the lookout for signs of infection, such as fever, chills and unusual discharge, and you should contact your doctor immediately if you develop these symptoms.
Cold Cone Biopsy as alternative treatment to KEEP
A cold cone biopsy is a surgical procedure that involves the removal of a tissue sample from the cervix, which is the lower portion of the uterus that exits into the vagina.
There may be precancerous cells or cancerous abnormal cells in the cervix. These cells are examined for indications of cancer using a cold cone biopsy.
Surgical removal of all afflicted tissue can also serve as a treatment.
How are cold cone biopsies performed?
A scalpel is used to do a cold cone biopsy since it is a sharp instrument. The cervix is opened up and a tiny cone-shaped sample of tissue is taken. The material is delivered to a lab for microscopic examination.
The hospital or surgical facility is where the procedure is carried out. Regional anesthesia (simply numbing the area) or general anesthesia (falling asleep and being pain-free) are both used.
In order to observe the cervix more clearly, the doctor inserts a device (a speculum) into the vagina1. Next, use the scalpel to cut away the tissue.
In order to collect more cells for analysis, the cervix’s canal may occasionally be scraped over the biopsy cone. Endocervical curettage (ECC) is what is used for this.
What precautions must be taken following a cold cone biopsy?
Some symptoms, including bleeding, spotting, cramps, or vaginal discharge, are common following a cold cone biopsy. Medications or cold compresses can help with these symptoms, which often last a few weeks.
Until your doctor instructs you to, you should postpone having sex, using tampons or douching. This promotes recovery and infection prevention.
Observe the doctor’s advice for follow-up and further checks. Depending on the biopsy’s results, additional examinations or medical care may be required.
Interesting facts and examples
Cold cone biopsy is a safe and effective procedure, but it may have some risk factors or complications, such as heavy bleeding, infection, narrowing of the cervix, or problems getting pregnant. These risks are rare and can be prevented or treated with the help of your doctor.
Cold cone biopsy can affect fertility or pregnancy in some cases. For example, if a lot of tissue is removed from the cervix, there may be an increased risk of preterm labor or miscarriage. That’s why it’s important to talk to your doctor about your reproductive plans before and after the procedure.
A cold cone biopsy is different from other ways of doing a cone biopsy, such as the LEEP procedure or laser beam. These forms use heat or light to cut the tissue, while the cold cone biopsy uses a scalpel. The doctor will choose the most appropriate form according to each case.
A cold cone biopsy is not the same as a Pap smear. A Pap test is a test done to look for abnormal cells on the cervix, but it doesn’t remove or test them further. A cold cone biopsy is done when the Pap smear shows abnormal cervical cells or is suspicious for developing cervical cancer. Cold cone biopsy allows you to confirm or rule out the diagnosis of cancer and see how advanced it is.
LEEP vs Cold Cone Biopsy
According to one study, patients with cold knife cone biopsy were significantly older than patients with LEEP (38 vs. 31 years, p=0.0001).
LEEP was associated with more tissue fragmentation (45.2% vs. 8.5%, p=0.0001) and uninterpretable surgical margins than cold knife cone biopsy (10.4% vs. 2.7%, p=0.001).
LEEP and cold knife cone biopsy had a similar rate of positive surgical margins.
In 24 cases, the sample obtained by LEEP or cold knife cone biopsy was negative for dysplasia (6.3%, 24/380), and the negative rates were similar between the LEEP and cold knife cone biopsy groups (6.8% vs. 5.6%, p=0.67).
Review of the previous biopsy or cytology of the 24 negative cases confirmed high-grade squamous intraepithelial lesion (HSIL/CIN2+) in 22 cases, and the remaining 2 cases were misinterpretations of low-grade squamous intraepithelial lesion (LSIL/CIN1). on biopsy or cytology.
The recurrence/residual rate for Cervical Intraepithelial Neoplasia was only 2.9% (11/373).
Hysterectomy for Cervical Intraepithelial Neoplasia
What is cervical intraepithelial neoplasia (CIN)?
CIN is a precancerous lesion that affects the cervix, the lower part of the uterus that connects to the vagina. CIN is caused by persistent infection with the human papillomavirus (HPV infection), which is transmitted through sexual contact. HPV infection is very common and most people eliminate it naturally, but in some cases, it can cause the appearance of abnormal cells in the cervix that can lead to cancer if not treated early.
What is a hysterectomy and why is it done for CIN?
The uterus, as well as occasionally the ovaries and fallopian tubes, are removed during a hysterectomy. When there are high risk factors of cancer progression or when conservative therapy (such local excision of lesions) are ineffective or impractical, a hysterectomy is performed for CIN. The only effective treatment for CIN and cervical cancer is hysterectomy, however it also results in fertility loss and has potential side effects such bleeding, infection, harm to other organs, or early menopause.
What was found in a recent study?
242 patients with a mean age of 46 years were included. 90% of them had high-grade CIN (NIC 2 or 3) and 10% had low-grade CIN (NIC 1). 60% of the patients had previously received one or more conservative treatments without success. 40% of the patients opted for hysterectomy as the first therapeutic option for different reasons, such as advanced age, desire for sterilization, comorbidities, or personal preference. The most frequent type of hysterectomy was laparoscopic (64%), followed by abdominal (28%) and vaginal (8%). The mean hospitalization time was 3 days and the mean follow-up time was 36 months.
The results of the study showed that:
- LT due to CIN increased significantly from 0.46% in 2010 to 3.32% in 2020, which could be due to a greater diagnosis of CIN due to the use of the HPV test as a screening method or to a greater demand for hysterectomy by patients.
- The rate of postoperative complications was low (4%), the most frequent being bleeding and infection. There were no deaths or reoperations related to hysterectomy.
- The CIN recurrence rate after hysterectomy was nil (0%), confirming the efficacy of this procedure in preventing cervical cancer.
- Patient satisfaction rate with hysterectomy was high (94%), although 18% reported decreased health-related quality of life. The factors that influenced satisfaction were age, the type of hysterectomy, the reason for the choice, and the histological result.
- The histological analysis of the surgical specimens revealed that 13% of the patients had a more serious than expected lesion (microinvasive or invasive cancer), which suggests the need to improve preoperative diagnosis and multidisciplinary management of these patients.
Conclusions
- Hysterectomy is a safe and effective therapeutic option for CIN, especially for patients who do not respond to conservative treatments or who prefer a definitive solution.
- Hysterectomy has a high degree of satisfaction among patients, although it can affect quality of life due to loss of fertility and early menopause.
- Hysterectomy should not be considered as an alternative to cervical cancer screening but as a resource for patients with high-risk CIN or with difficulties in accessing conservative treatments.
- Hysterectomy should preferably be performed laparoscopically since it offers advantages such as less bleeding, less pain, less hospitalization time and better recovery.
- More research is needed to evaluate the factors that influence the decision of patients to opt for hysterectomy and to improve their selection and follow-up criteria.