Life after Hysterectomy: What fills the space?
Introduction
Definition of Hysterectomy
Hysterectomy is among the most frequent gynecological surgeries that involve the removal of a woman’s uterus. It is performed to treat various illnesses where its various types are selected for specific patient cases. Furthermore, there exist different surgical techniques for performing the operation, depending on the patient’s health, age and general condition.
Common reasons for a Hysterectomy
Hysterectomy is recommended to women with various common conditions. Uterine fibroids, endometriosis, abnormal uterine bleeding, uterine prolapse, adenomyosis, chronic pelvic pain, and cancer in the uterus, ovaries or cervix are among the typical reasons for requiring a hysterectomy. Some additional factors that may necessitate a hysterectomy include chronic pelvic infections or a serious condition of pelvic inflammatory disease.
Types of Hysterectomy
Total hysterectomy
Is a treatment in which the uterus and cervix are both taken out of the body. This kind of hysterectomy is typically carried out to cure uterine cancer, stop cancer from spreading to the cervix, or stop persistent cervicitis inflammation. Major surgery like a total hysterectomy has a longer recovery period than other procedures.
Partial hysterectomy or supracervical hysterectomy
Only the upper section of the uterus is removed with this type of hysterectomy also known as subtotal or supracervical hysterectomy. The cervix is left in place, which shortens the recovery period and preserves the patient’s hormonal function. However, if the patient has a history of cervical dysplasia or malignancy, Partial hysterectomy surgery is not suggested.
Radical hysterectomy
A radical hysterectomy is a more invasive procedure performed when cancer is present in the uterus or cervix. It involves removing not just the uterus but also the surrounding tissues, such as the ovaries, fallopian tubes, upper part of the vagina and lymph nodes. This procedure has a higher risk of complications and requires a longer recovery period.
Surgery Techniques
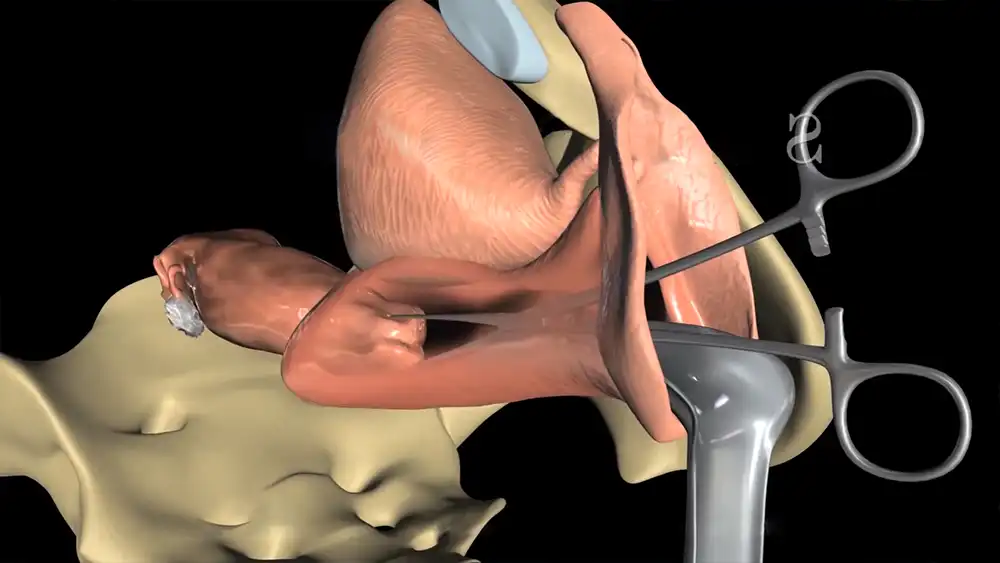
Abdominal hysterectomy

Abdominal hysterectomy is the most common technique used to remove the uterus, and involves making an incision in the lower abdomen. This type of hysterectomy is usually recommended when there are large fibroids present, or any adhesions in the area. It may also be used if other organs or tissues need to be removed during the surgery. An overnight hospital stay is likely necessary after this procedure, and recovery typically takes about four to six weeks for full healing.
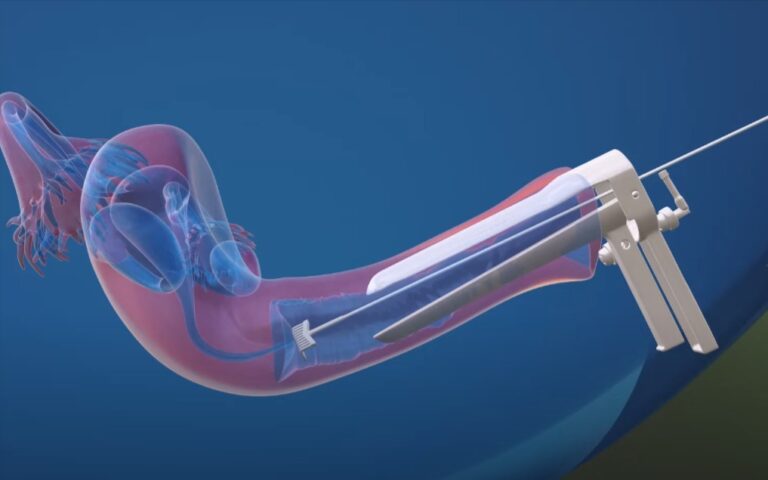
Vaginal hysterectomy
Vaginal hysterectomy is another procedure that involves removing the uterus through the vagina without any external incisions. This requires surgery with a lighted instrument called a hysteroscope and is generally less invasive than abdominal hysterectomy. However, this method can only be used in select cases where the uterus is small and easily accessible through the vagina. Recovery time for vaginal hysterectomy typically varies between 6-8 weeks.
Laparoscopic hysterectomy
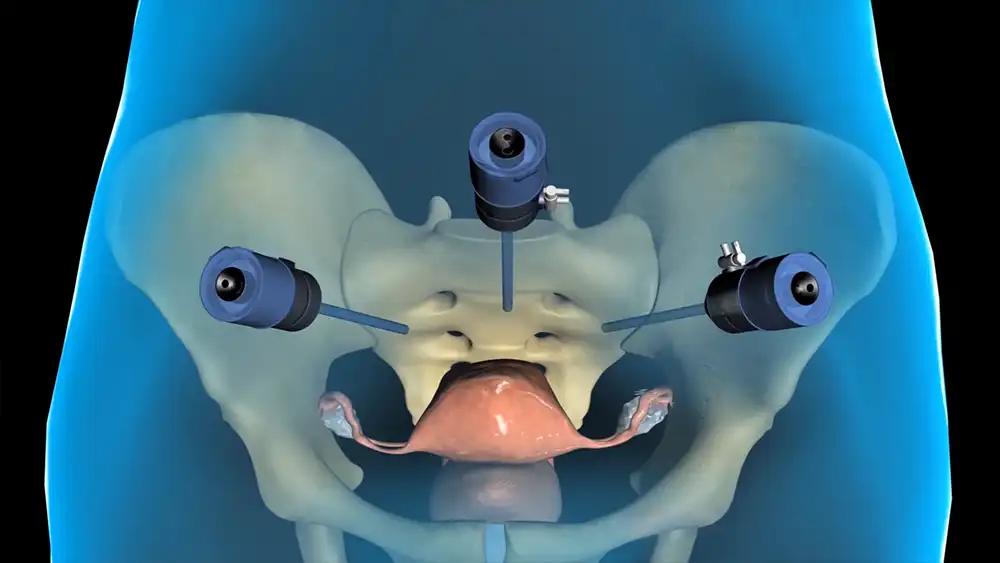
Laparoscopic hysterectomy is a minimally invasive technique that uses small incisions in the abdomen to insert a camera and surgical instruments to remove the uterus. This approach offers many benefits such as reduced blood loss during surgery, smaller incisions, and less postoperative pain. Moreover, laparoscopic hysterectomy usually requires a shorter hospital stay and faster recovery time compared to other techniques.
Robotic assisted laparoscopic hysterectomy
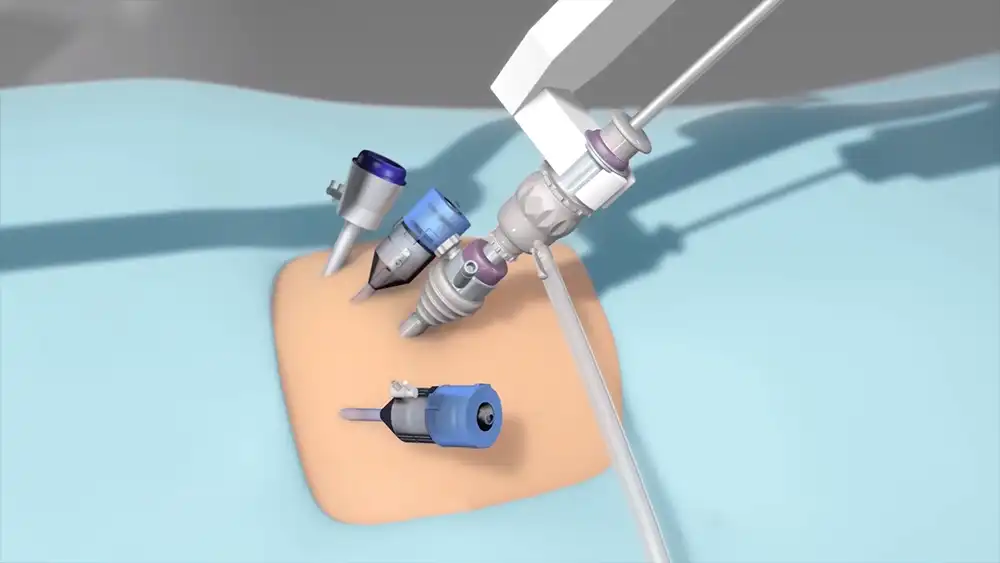
This procedure uses robotic arms to facilitate delicate maneuvers through small incisions in the abdomen, resulting in a number of advantages over traditional hysterectomies. Benefits of robotic hysterectomy include less blood loss during surgery, shorter hospital stays and quicker recovery times, as well as fewer complications and improved precision. Furthermore, it allows surgeons to carry out complex abdominal surgeries with greater accuracy than when using traditional methods.
What happens after a Hysterectomy
Physical changes after a Hysterectomy

Following the procedure, a woman may experience pain and discomfort, as well as fatigue due to the healing process. Hormonal changes can also occur, leading to hot flashes, night sweats, and mood swings. In addition, depending on the type of hysterectomy performed, the patient may experience vaginal dryness, urinary incontinence, or muscle weakness in her abdomen. While these physical effects can be uncomfortable and disconcerting, many women report feeling relief after their surgery for disorders such as endometriosis or fibroids.
Emotional changes after a Hysterectomy
The emotional changes that come with a hysterectomy can vary from woman to woman. Some may feel positive emotions like relief and happiness, while others may experience sadness or grief due to the loss of their reproductive capabilities. Women may also struggle with anxiety about how the surgery will impact their physical health and appearance, as well as how it will affect their relationships with their partners or spouses.
What to expect during recovery

During recovery from a hysterectomy, it is normal to experience some pain and discomfort as your body heals. Generally, you should expect to take several weeks to recover, during which time it is important to follow your doctor’s instructions for proper rest and nutrition as well as for managing any pain. Women should also avoid placing strain on their abdomen by lifting heavy items or engaging in physical activities until at least six weeks after the procedure. Additionally, fatigue may be common due to the healing process, so it’s important to pace yourself and allow yourself ample time to rest and replenish.
After a Hysterectomy what fills the space?
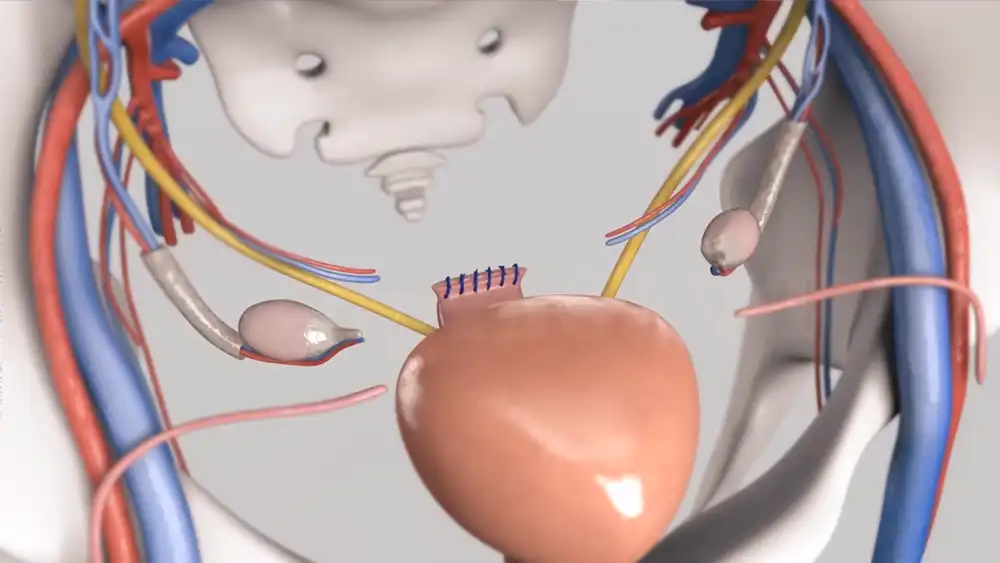
After a hysterectomy, the space inside the abdomen will be filled with internal scar tissue, as this is the body’s natural healing process. As scar tissue forms in the area where the uterus was removed, it can help to reduce bleeding and provide support for surrounding organs. It also helps to create a barrier between abdominal contents, reducing damage or pain when manipulating or extending other organs in the area. In some cases, your doctor may opt to insert an additional material such as mesh to help support surrounding organs and reduce risk of tissue separation following a hysterectomy.
The role of the pelvic floor muscles
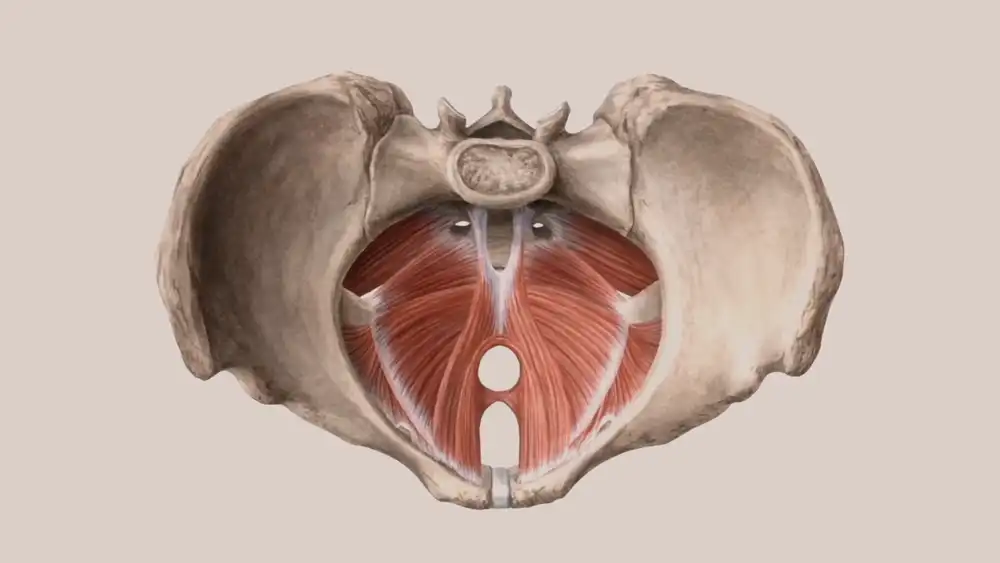
These muscles play a vital role in providing support and stability to the pelvic organs. These muscles work to help keep contents of the abdomen from spilling into the pelvic cavity, as well as providing structural support for organs such as the bladder and rectum. In addition to providing physical support, they also help to control urinary incontinence and may even help with sexual function. Regular exercise of these muscles can be beneficial before and after surgery. Pelvic floor exercises like Kegels strengthen these important muscles, leading to improved overall health outcomes following a hysterectomy.
How the body adapts to the absence of the uterus
The space inside the abdomen will be filled with scar tissue as part of this healing process, providing support for surrounding organs and reducing the risk of damage or pain when manipulating or extending them. Over time, hormonal imbalances may occur as a result of the uterine removal, leading to symptoms like hot flashes and night sweats. These can often be managed with medication and lifestyle changes. Additionally, physical changes may occur due to loss of estrogen such as thinning hair and dry skin.
Changes in bladder and bowel function
As pelvic floor muscles are weakened, it is possible that there may be more frequent and urgent trips to the bathroom. Women might also experience stress incontinence, leading to leakage of urine when sneezing or coughing. Additionally, constipation can also be an issue as both estrogen and progesterone play important roles in helping food move through the bowels. Regular exercise routines and increased fiber intake can help alleviate some of these issues.
The impact of Hysterectomy on sexual function
While this surgical procedure is typically performed to alleviate pain, it can have an impact on sexual function. During the procedure, the uterus and cervix may be partially or completely removed, along with surrounding tissues that control lubrication and vaginal tension. Without these structures present, it is common for women to experience less sensation during sexual intercourse as well as decreased arousal and vaginal dryness. However, estrogen supplements and other treatments may help reduce some of these symptoms. It is also important to remember that many women find their sex life improving once hormonal imbalances are addressed and post-operative pain subsides.
Risk of Pelvic Organ Prolapse
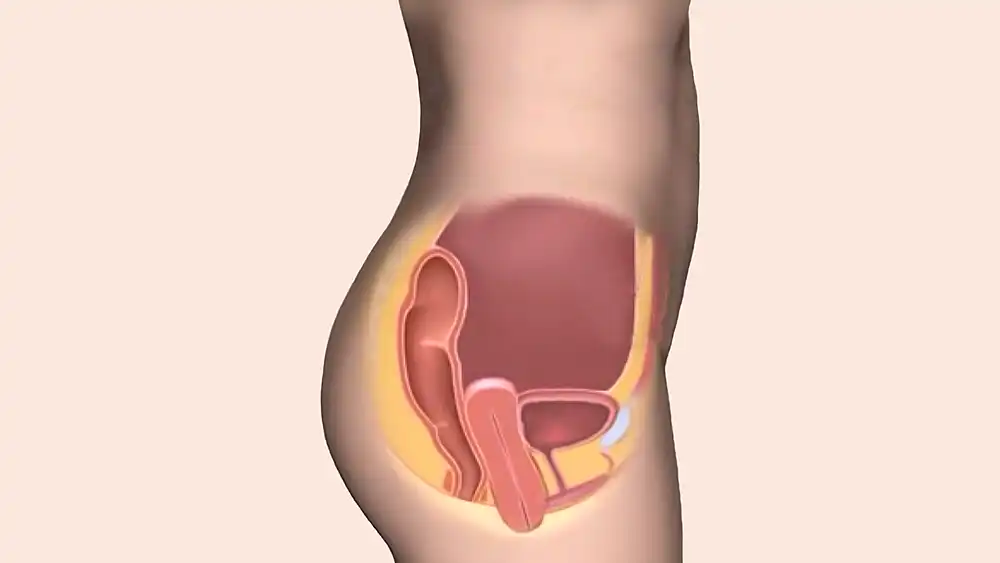
Women who have had a hysterectomy are more likely to develop Pelvic Organ Prolapse. The uterine prolapse happens when the uterus falls into or out of the vaginal opening. When the upper region of the vagina slides down and out of the body this is known as vaginal vault prolapse. The prolapse or lowering of the bladder into or outside of the vagina (cystocele) is referred to as bladder prolapse. A woman’s susceptibility for this illness is increased by the weaker pelvic floor muscles caused by a hysterectomy. If you have any symptoms, such as feeling pressure in your pelvic area or spotting a protrusion inside your vagina, you should consult your doctor.
Coping mechanisms for the changes
It’s important to give yourself time to adjust and to seek out support from family, friends, and healthcare providers if needed. Exercise is also an effective way to help keep both physical and mental health in check during recovery. Regular physical activity not only helps strengthen muscles, bones and joints, but can also improve mood and provide stress relief. Additionally, eating a healthy diet full of fruits and vegetables can boost energy levels as well as physical and emotional wellbeing. Finding activities that you enjoy such as hobbies or creative pursuits can also help you cope with changes after a hysterectomy.
Pelvic Floor Health after Hysterectomy
Understanding the pelvic floor muscles
These muscles stretch from the pubic bone to the tailbone, supporting vital organs like the bladder, uterus, rectum and small intestine. Not only do these muscles help with bladder and bowel control, but also sexual functions like orgasm. If weakened, these muscles can prevent you from having full control over when you urinate or defecate. In more severe cases, pelvic organs may prolapse with means to drop downwards into the vagina or outside due to weakened pelvic floor muscles. Additionally, issues such as anal and vaginal problems, pelvic pain and discomfort can be caused by weak pelvic floor muscles.
Pelvic floor problems after Hysterectomy
Hysterectomy can have a wide-ranging impact on pelvic floor health. In some cases, the temporary weakening of the pelvic floor muscle can lead to immediate issues such as bladder leakage and decreased strength in other pelvic organs. Long-term effects may include difficulty in passing stools, pain during intercourse and further discomfort from weakened muscles. Additionally, menopause which is often associated with hysterectomy may also contribute to pelvic floor weakness due to changes in hormones that affect these muscles as well as general loss of muscle mass.
Pelvic floor exercises to improve strength and function
Pelvic floor exercises can help improve strength and function of the pelvic floor muscles. These exercises include targeted contractions, using Kegels to strengthen and relax the pelvic muscles. Regular and consistent practice of these exercises may help with bladder leakage, rectal incontinence, as well as sexual response by increasing sensation and improving the ability to contract during orgasm. Depending on severity of symptoms, physical therapy may need to be included but it is important to note that pelvic floor muscle training is not always a sufficient solution and so further treatments such as medication or surgery may need to be considered.
Preventing pelvic organ prolapse
Preventing this condition requires taking steps to promote good health and strengthen your pelvic floor muscles. This can include making lifestyle changes like eating a balanced diet, staying active, and quitting smoking. Pelvic floor exercises are also important for strengthening those muscles and providing extra support for other abdominal organs. Additionally, wearing comfortable clothing and avoiding lifting heavy objects is recommended to reduce the risk of pelvic floor problems that could incite prolapse.
Hormonal Changes after Hysterectomy
Understanding the role of hormones in the body
Hormones play a critical role in the body and are involved in many of its processes. Hormones are chemical messengers that are produced by glands in the endocrine system. They travel through our bloodstream to various organs and regulate various functions, such as metabolism, reproduction, and growth. When hormones become unbalanced due to disease or lifestyle factors, it can have far-reaching consequences for our overall health.
How Hysterectomy affects hormonal balance
Depending on the type of surgery performed, a partial, complete, or radical hysterectomy may have varying effects on hormone balance. While total and radical hysterectomies remove all or part of the uterus along with the cervix and may also remove the ovaries if clinically necessary, partial hysterectomies just remove a section of the uterus and normally do not affect ovarian function. In these circumstances, the uterus and ovaries both stop producing hormones, which causes an imbalance in hormones like progesterone and estrogen. In order to improve health and lessen stress on the pelvic floor muscles after a hysterectomy, lifestyle modifications like regular exercise, eating a balanced diet, quitting smoking, and wearing supportive clothing can all be helpful.
Hormone replacement therapy (HRT) options

Hormone replacement therapy (HRT) is a common treatment for those experiencing hormone imbalance due to certain medical conditions. It is typically used to supplement the body’s natural hormones, and can be administered in many different ways. Options range from oral medications like pills, to topical products such as lotions, patches and gels. In some cases, hormone injections may also be used. In order to determine the safest and most effective course of action, it is best to consult with a doctor who specializes in HRT.
Navigating Menopause after Hysterectomy
Early onset of menopause
It is possible to experience early onset menopause after a hysterectomy, although it is not as common as going through natural menopause at the usual age of 50 or older. Early onset of menopause after hysterectomy can be caused by the removal of part or all of the ovaries during surgery. The treatments for early onset menopause after hysterectomy are similar to those used for naturally occurring menopause and may involve lifestyle modifications such as exercising regularly, eating a healthy diet and reducing stress levels. Hormone replacement therapy (HRT) may also be recommended in order to provide relief from more severe symptoms.
Symptoms of menopause after Hysterectomy

Symptoms of menopause after a hysterectomy can vary significantly depending on the individual and the extent to which their ovaries were removed. Common symptoms may include hot flashes, night sweats, mood swings and sleep disturbances. Other physical signs such as thinning hair, vaginal dryness and irregular periods may also occur due to the drop in hormone levels caused by the surgery. The severity of these symptoms may depend on whether or not the woman’s ovaries have been completely removed during the procedure.
Coping mechanisms for menopause symptoms
For physical symptoms such as hot flashes, night sweats and disrupted sleep, reducing stress levels and exercising regularly can be helpful in providing relief. Eating a balanced diet with foods that are rich in omega-3 fatty acids, calcium, magnesium and vitamin E may also assist with providing symptom relief. Hormone replacement therapy (HRT) is another option for those experiencing severe symptoms, however it should only be used after consulting with your doctor. Other techniques such as acupuncture or yoga may provide further relief from menopausal symptoms depending on the individual’s situation.
Coping with Emotional Changes after Hysterectomy
Addressing feelings of loss and grief
Experiencing feelings of loss and grief after a hysterectomy is common and normal. It is important to be kind to yourself during this difficult time and reach out for help if needed. It can also be helpful to practice self-care, such as getting enough rest, eating healthy foods, exercising regularly and doing activities that you enjoy.
Seeking support from loved ones and professionals
Seeking out support from family and friends can be extremely beneficial in providing emotional relief and coping with the adjustment period. Having open conversations with loved ones about your experience may provide comfort during times of distress. Professional counseling services or joining a support group may also be beneficial for gathering resources and guidance as you move through recovery.
Tips for managing emotional changes
Here are some tips for coping with these changes:
- Talk openly about your experience with family and friends for emotional support.
- Seek professional counseling services or join a support group for additional guidance during the adjustment period.
- Practice self-care by getting enough rest, eating nutritious meals, exercising regularly, and doing activities that bring you joy.
- Consider holistic approaches such as journaling, yoga or mindfulness to help manage stress and emotions.
- Remember to be kind to yourself and be patient as you move through recovery.
The Impact of Hysterectomy on Fertility
Permanent infertility after Hysterectomy
Undergoing a hysterectomy often comes with permanent infertility due to the tissue responsible for bearing children being removed during the surgery. In some cases, it may still be possible to carry a child if the ovaries are left intact, but this will depend on the individual’s age and overall health.
Options for fertility preservation before Hysterectomy
For those considering undergoing a hysterectomy, there are options available for preserving fertility prior to surgery. Embryo cryopreservation (freezing fertilized eggs) and ovarian tissue cryopreservation (freezing ovarian tissue) are two potential methods of preserving potential fertility before undergoing a hysterectomy. These treatments allow women who want to bear children in future to store their eggs or ovarian tissue for later use.
Maintaining a Healthy Lifestyle after Hysterectomy
The importance of physical activity after Hysterectomy
Physical activity helps promote healing and build strength while lessening pain, fatigue, and stiffness. Aerobic activities like walking and swimming help to increase energy levels and improve circulation which can reduce swelling. Strengthening exercises such as yoga and weight lifting can strengthen the abdominal muscles that have been weakened by the hysterectomy to help you regain balance and stability during movement.
It is important for individuals to listen to their bodies during their recovery period after a hysterectomy, as this will help them determine what types of physical activities will work best for them. If unsure, it is advisable to start with low-intensity activities such as stretching or gentle walking before progressing to more vigorous forms of exercise.
Healthy diet choices after Hysterectomy
After a hysterectomy, a diet rich in fruits and vegetables can help restore energy levels, improve overall health, and reduce fatigue. Incorporating protein-rich foods such as meats, eggs, nuts, and lentils into one’s diet provides vital nutrients for the body’s regeneration processes. Incorporating complex carbohydrates such as quinoa and brown rice into one’s diet is advantageous for supplying additional energy and fiber to promote a sensation of satiety and providing the body with essential vitamins, minerals, and fiber. To prevent mood swings, it is essential to limit the consumption of processed foods with high levels of saturated fat. Consuming copious amounts of water throughout the day helps maintain hydration.
Complications and Risks after Hysterectomy
Potential complications after Hysterectomy
- Infection
- Heavy blood loss
- Reactions to anesthesia
- Damage to nearby organs or tissue.
- Pain during sexual intercourse
- Bladder problems due to weakened muscles
- Changes in hormone levels leading to menopausal symptoms such as hot flashes and night sweats.
After the procedure, one should monitor for signs of infection such as a fever with chills or a foul-smelling discharge from the incision site. In extreme cases, further medical attention may be necessary if complications arise.
How to reduce risks and complications
Select an experienced and qualified doctor who is up-to-date with the latest medical advancements and treatments, as well as one who takes their time to discuss all potential risks in detail. The patient should also be honest about their medical history, including any previous surgeries or other gynecological conditions.
Once the surgery is scheduled, it is important for the patient to follow all pre-operative instructions, such as fasting before surgery or stopping certain medications beforehand, to ensure a successful operation with minimal side effects.
Finally, following post-surgery instructions such as avoiding heavy lifting and wearing supportive garments can reduce chances of complications and promote an optimal recovery period.
Life Expectancy and Hysterectomy
A hysterectomy may affect a person’s life expectancy in both positive and negative ways. On the one hand, uterine removal may reduce the risk of ovarian cancer, cervical cancer, and uterine fibroids. This could result in an extended life expectancy. On the other hand, there are potential long-term risks to consider, such as pain during sexual activity or bladder difficulties as a result of the surgery-caused muscle weakness.
In addition, hormone changes following a hysterectomy may result in premature menopause symptoms, which may increase the associated health risks, such as heart disease and stroke. Ultimately, a person should discuss any potential long-term hazards with their physician in order to make an informed decision regarding their health care and to ensure that they are taking measures to maximize their life span.
FAQs
How long does recovery from a hysterectomy take?
Recovery time for a hysterectomy can vary depending on the type of procedure that was performed and individual factors such as age and overall health. Generally speaking, full recovery may take up to 6 weeks or more.
What kind of follow-up tests or care might be required after surgery?
After a hysterectomy, you may need regular annual follow-ups with your gynecologist including physical exams, blood tests and ultrasounds if necessary. In addition, emotional counseling may also be beneficial in order to cope with any changes in lifestyle due to this operation.
Can infertility still occur after a hysterectomy?
If only the uterus is removed during the procedure (known as subtotal/partial hysterectomy), then infertility is not an issue since eggs are still present in the ovaries and can still be fertilized by sperm. However, if both organs are removed (total hysterectomy) then yes, infertility will occur since eggs are no longer present in the body.
Will there be a noticeable weight change after a hysterectomy?
Yes, some individuals experience weight fluctuation due to hormonal changes caused by removal of uterus/ovaries during this procedure; however diet modification coupled with regular exercise can help control hormone levels while aiding in successful weight management over time..
Are there any foods I should avoid eating after my surgery?
Certain foods known to cause digestive distress like high sugar foods/beverages, spicy food items & fried fats should generally be avoided until full recovery prior indulging in them again at moderate quantities; although individual dietary preferences may depend on personal preference & medical condition(s).
Conclusion
In summary, hysterectomies can have a profound effect on a woman’s life, both physically and emotionally. The procedure comes with potential risks and side effects that should be carefully considered before undergoing the operation. It is also essential to take appropriate measures after the surgery such as regular follow-up appointments with your doctor, avoiding strenuous activity and monitoring for any changes in health or emotional status.