Do you need a Radical Hysterectomy for Cervical Cancer?

Cervical cancer typically occurs in the cervix, which is the lower portion of the uterus that links to the vagina. Hysterectomy is a surgical procedure that removes the uterus along with the ovaries and fallopian tubes. This disease constitutes one of the primary reasons for a hysterectomy, especially among those diagnosed during the early stage cervical cancer. Hysterectomy may also be considered as a preventive measure for individuals at a high risk of developing cervical cancer, such as those with a prior history of abnormal cervical cells or HPV infection. Women should undergo regular Pap tests and follow-up care to facilitate the detection and possible prevention of cervical cancer while discussing potential treatments with their healthcare provider.
Understanding Cervical Cancer
What causes cervical cancer?
Cervical cancer usually stems from human papillomavirus (HPV) infection, which is a commonly transmitted sexually transmitted illness. While most women infected with HPV do not develop cervical cancer, changes to the cells of the cervix can occur in some cases and potentially lead to cancer over time. Smoking, weakened immune systems, and a history of sexually transmitted diseases are also contributing risk factors for cervical cancer. Illness prevention should involve regular Pap tests for cervical cancer screening and addressing any symptoms or concerns with healthcare providers. Those at risk of HPV infection can receive HPV vaccines. Understanding cervical cancer causes can help individuals to take a proactive approach to prevention while promoting early detection and treatment.
Signs and symptoms of cervical cancer
Early stage cervical cancer is one of the most treatable types of the disease, but it can only be found through regular screenings and Pap tests. In its early stages, cervical cancer usually doesn’t show any outward signs. This is why Pap tests are so important for finding any abnormalities that could be signs of the disease. Abnormal vaginal bleeding, such as bleeding during periods, after sex, or after menopause, is the most typical sign. Pelvic pain, discomfort during sexual activity, and unusually colored or scented vaginal discharge are further signs of cervical cancer. Even if they appear minor or uncommon, it’s crucial to see a doctor if you encounter any of these symptoms. Maintaining regular gynecologic examinations and sharing any potential concerns with a healthcare professional are critical since early detection of cervical cancer is essential for successful treatment.
Stages of cervical cancer
Cervical cancer is typically classified into four stages, depending on how far the cancer has advanced.
- Stage 0 – Implies that the cancer is localized to the surface layer of the cervix and has not yet infiltrated deeper tissue.
- Stage I – Cancer has penetrated beyond this superficial layer and invaded more internal layers of the cervix.
- Stage II – It’s spread to nearby tissue such as the upper part of the vagina or tissues surrounding the cervix.
- Stage III – It has extended to lower parts of the vagina or pelvic wall and may have also caused a blockage in ureters- tubes connecting kidneys to bladder.
- Stage IV – Refers to spreading of cancer beyond these areas, potentially infiltrating other organs like lungs or liver.

Identifying which stage cervical cancer is in can help determine treatment options; usually, early stage cervical cancer require less aggressive measures. Henceforth, regular Pap tests and check-ups are encouraged for timely detection and cure before it spreads further.
Overview of non-surgical cervical cancer treatment options
Non-surgical treatments for cervical cancer can be just as effective as surgery in many cases. Radiation therapy is the most commonly used option, and it works by destroying cancer cells while preserving healthy tissue. Depending on the stage and size of the tumor, chemotherapy may also be an option. For early stage cervical cancer or small tumors, cryotherapy (freezing) or conization (removal of a cone-shaped section of the cervix) may be options to consider.
When is hysterectomy recommended for cervical cancer?
Stage of Cancer
When it comes to the treatment of cervical cancer, the stage at which it is detected is an important factor in deciding whether a hysterectomy is necessary. In very early cervical cancer, other treatments such as surgery or radiation may be recommended, while more advanced cases may require a hysterectomy to remove the cancer and prevent its spread.
Size of Tumor
The size of the tumor is another important factor in deciding whether a hysterectomy is necessary. If the tumor is small, a cone biopsy can be performed to remove it. However, if the tumor is large or has spread to other areas, a hysterectomy may be the best course of action.
Age and Health
Age and health status are significant factors to consider when determining whether or not a hysterectomy is necessary for the treatment of cervical cancer. Younger women who have intentions of starting a family in the future can explore alternative treatments such as surgery or radiation therapy, while older women who have completed their families may opt for a hysterectomy in order to prevent further spread of the cancer.
Minimally Invasive Radical Hysterectomy or Radical Abdominal Hysterectomy?
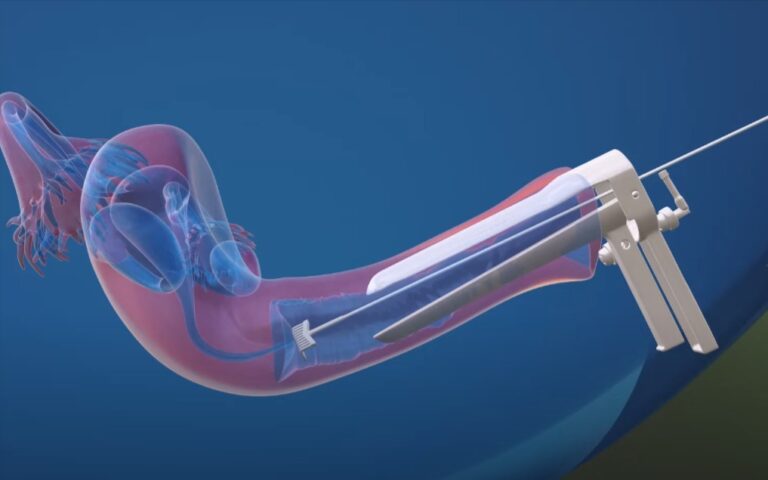
Minimally Invasive Radical Hysterectomy
A minimally invasive radical hysterectomy involves the removal of the cervix and uterus. The cervix and uterus are removed laparoscopically, which involves making tiny incisions in the abdomen so the surgeon can insert small instruments. This is a minimally invasive surgery in comparison to an abdominal hysterectomy, resulting in a shortened recovery period, less pain, and fewer scars.
Recovery time is one of the most significant advantages of a minimally invasive radical hysterectomy. This procedure typically results in less discomfort and a quicker return to normal activities than an abdominal radical hysterectomy.
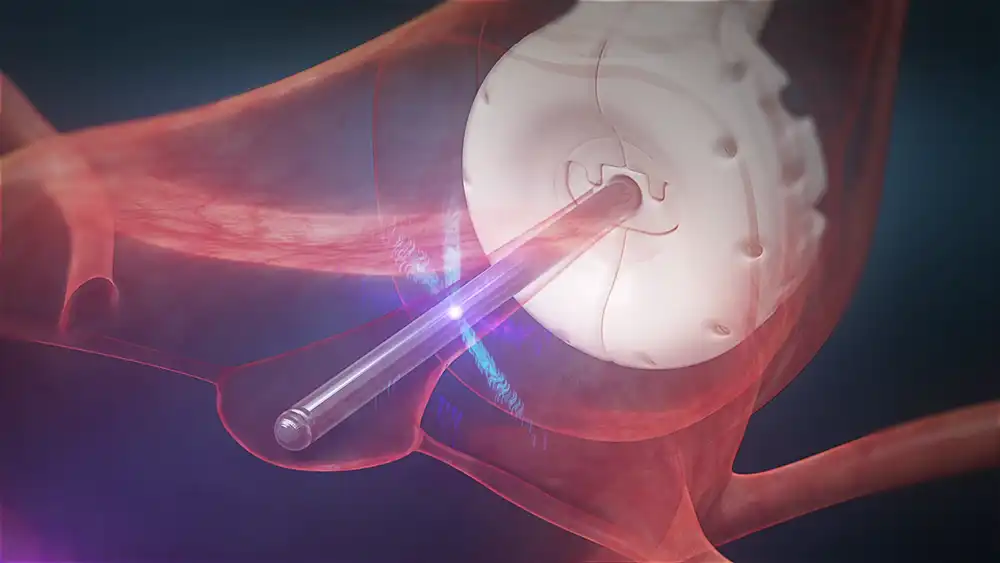
Abdominal Radical Hysterectomy
The cervix and uterus are extracted through a larger incision in the abdomen during a radical hysterectomy. This procedure is more invasive than a minimally invasive radical hysterectomy, so the recovery period is prolonged, and there is more pain and scarring.
Longer recovery time is one of the most significant drawbacks of an abdominal radical hysterectomy. Patients who undertake this procedure typically experience more discomfort and are unable to resume normal activities as quickly as those who undergo a minimally invasive radical hysterectomy.
Comparison
There are a number of distinctions to be made between an abdominal radical hysterectomy and a minimally invasive radical hysterectomies when doing a comparison of the two procedures. The length of the incision, the amount of time needed for recuperation, the level of discomfort, and the likelihood of scarring are some of these aspects.
Even though it is less invasive than an abdominal radical hysterectomy, a radical hysterectomy that is performed using minimally invasive techniques might not be the right choice for every patient. For patients who have advanced cervical cancer or bigger uteruses, an open radical hysterectomy may be required in addition to a standard hysterectomy in order to eliminate every trace of the disease.
How to Prepare for an Abdominal Radical Hysterectomy
Understanding the Procedure
Before you undergo a radical hysterectomy, it’s essential to understand what the surgery involves. You should discuss the procedure with your doctor and ask any questions you may have. It’s also helpful to research the procedure online or through reputable sources. Understanding the surgery and its potential risks and benefits can help you make an informed decision.
Meeting with Your Healthcare Team
A radical hysterectomy is a complex procedure that requires a team of healthcare professionals. Before your surgery, you will likely meet with your surgeon, anesthesiologist, and other members of your healthcare team. These meetings are an opportunity to discuss any concerns you may have, provide your medical history, and review any medications you are taking. Your healthcare team will also give you specific instructions on how to prepare for the surgery, including fasting guidelines and medication management.
Making Lifestyle Changes
Making lifestyle changes before surgery can help improve your overall health and increase your chances of a successful outcome. Your doctor may recommend that you quit smoking and limit alcohol consumption. You may also need to make changes to your diet and exercise routine. Maintaining a healthy lifestyle can help improve your immune system and decrease the risk of complications during surgery.
Preparing Your Home
After surgery, you may need to spend several days or weeks recovering at home. Before your surgery, it’s important to prepare your home to ensure a comfortable and safe recovery. This may include arranging for a caregiver or family member to assist you with daily tasks, such as cooking, cleaning, and personal care. You may also need to make modifications to your home, such as installing grab bars in the bathroom or rearranging furniture to accommodate mobility aids.
Packing for the Hospital stay
Before your surgery, you will need to pack a bag for your hospital stay. Your healthcare team will provide you with a list of items to bring, which may include comfortable clothing, toiletries, and entertainment such as books or music. You should also bring any medications you are taking and provide your healthcare team with a complete list of all medications and supplements.
Understanding the Recovery Process
Recovering from a radical hysterectomy can take several weeks or months, depending on the extent of the surgery and your overall health. It’s essential to understand the recovery process and what to expect. Your healthcare team will provide you with specific instructions on post-surgical care, including wound care, pain management and physical activity. It’s important to follow these instructions carefully and to attend all follow-up appointments with your healthcare team.
Managing Emotions
Having surgery can be an emotionally trying experience. It is essential to manage your emotions prior to and following surgery. This may involve obtaining support from friends and family or consulting a mental health professional. You may also benefit from practicing relaxation techniques like deep breathing and meditation.
Managing Possible Complications
The hazards associated with a radical abdominal hysterectomy include bleeding, infection, and blood clots. It is essential to discuss possible complications with your healthcare team and to be aware of warning indicators, such as fever or excessive bleeding. Contact your healthcare team immediately if you experience any symptoms or concerns.
Pros and Cons of Hysterectomy for Cervical Cancer
Benefits of hysterectomy for cervical cancer
Hysterectomy offers numerous benefits for the treatment of cervical cancer. It eliminates the need for aggressive radiation or chemotherapy treatments, allowing quicker recovery and fewer side effects. For many women, it is also curative; a hysterectomy can be effective at removing all traces of cancer from the body. Additionally, it can provide peace of mind by reducing the risk of recurrence or metastasis in cases where other treatments may not have been completely successful.
Risks and side effects of hysterectomy for cervical cancer
The primary risk associated with a hysterectomy is the potential for damage to surrounding structures. Another risk associated with a hysterectomy is the loss of fertility, as pregnancy is no longer possible following the procedure.
It is also important to note that if a woman has not already gone through menopause, she will immediately enter it following a hysterectomy; this may cause additional symptoms, such as hot flashes or night sweats. While these effects are often temporary, it is important for individuals to understand what steps they can take in order to manage them.
Additionally, some women may experience difficulty with bladder control after having a hysterectomy. Taking care to exercise regularly and using pelvic floor exercises can help reduce the risk of incontinence in some cases. Other common side effects include difficulty with sexual activity, fatigue, or depression.
How hysterectomy affects sex life and hormone levels
A hysterectomy can have significant implications for an individual’s sexual life and hormone levels. One of the primary effects is a decrease in estrogen production, resulting in changes to a woman’s sexual desire, interest and ability to experience pleasure. Furthermore, the removal of uterine tissue and internal reproductive organs may significantly alter how one experiences sexual sensations compared to before surgery; things like lubrication or stimulation might be different. Additionally, mood swings are also common due to fluctuating hormone levels from the surgery. Lastly, if both ovaries are removed during the procedure, menopause will occur immediately following the procedure; this may cause additional symptoms such as night sweats or hot flashes that need to be managed.
The emotional impact of having a hysterectomy
A hysterectomy can have a profound emotional impact on a woman’s life. It can be difficult to lose reproductive organs and the ability to conceive children. Additionally, pre-existing mental health issues such as anxiety or depression may worsen due to the physical and hormonal changes caused by the surgery. In some cases, patients experience feelings of grief, guilt and anger related to their inability to become pregnant or bear children. Some women may even feel a sense of loss for their femininity since hysterectomies can also influence hormones that are responsible for sexual behavior and libido. It is important that women know that it is normal to experience these emotions after a hysterectomy, and they should seek professional help if needed.
Alternatives to Hysterectomy for Cervical Cancer
Overview of non-surgical treatments for cervical cancer
While a hysterectomy is often the most effective treatment for cervical cancer, there are alternative non-surgical treatments for those who are not interested or unable to undergo surgery. Radiation therapy such as external beam radiotherapy may be used to treat early stage cervical cancer. In some cases, targeted chemotherapy drugs can be used to attack and kill cancer cells without damaging surrounding healthy cells. Immunotherapy is another option, which harnesses the power of one’s immune system to fight the disease. The availability of these treatments will depend on the stage of cancer, but they can provide an opportunity for patients to receive treatment without undergoing a hysterectomy.
Explanation of fertility-sparing treatments
In some cases, it is possible to treat cervical cancer while preserving fertility. Fertility-sparing treatments involve preserving both ovaries and the uterus, depending on the stage of the cancer. One option is a trachelectomy, which is a surgery that removes only the cervix and leaves the uterus intact for a quicker recovery than with a hysterectomy. This can help preserve fertility if the cancer has not spread beyond the cervix. Another alternative is chemo-radiation therapy, where chemotherapy and radiation therapy are employed at the same time to target and kill cancer cells without damaging surrounding healthy tissue. Furthermore, removing affected lymph nodes can prevent further spread of cancer cells and thus preserve fertility. By exploring all available fertility-sparing treatments, it may be possible to treat cervical cancer while still giving individuals an opportunity to have children in the future.
The effectiveness and limitations of alternative treatments
Alternate treatments for cervical cancer have been utilized for millennia, but their efficacy remains uncertain. Herbal remedies, dietary supplements, acupuncture, and cupping are among the treatments that have been used to treat the disease’s symptoms. Although anecdotal evidence suggests that these therapies may alleviate certain symptoms, the scientific evidence supporting their efficacy in curing cancer remains equivocal. In addition, alternative treatments typically lack regulatory oversight and should not be substituted for conventional medical treatments like radiation therapy or chemotherapy. Although complementary therapies may provide advantageous support when used in conjunction with conventional therapies, they should never be used as the primary treatment for cervical cancer.