Understanding Cervical Cancer and the Role of Hysterectomy
I. Introduction
A brief overview of cervical cancer and its prevalence
Cervical cancer is a type of cancer that develops in the cervix, the lower part of the uterus that connects to the vagina. It is the fourth most common cancer in women worldwide and a leading cause of death for women in developing countries. According to the World Health Organization (WHO) , there were an estimated 570,000 new cases and 311,000 deaths from cervical cancer in 2018.

Cervical cancer is preventable with vaccination and appropriate screening. Through vaccination, many types of HPV can be prevented from infecting the cervix and thus preventing cervical cancer. Cervical cancer screening can detect precancerous cells in the cervix, which can be treated before they develop into cancer.
Importance of early detection and treatment
Detection and treatment of cervical cancer at an early stage are crucial for the best potential prognosis. If cervical cancer is found in its early stages, it can be properly treated, and survival rates are substantially increased. Regular screenings, such as Pap smears, can detect abnormal cervical cells before they develop into cancer. Along with follow-up care and monitoring, these screening tests are essential for early detection of cervical cancer.
Importantly, cervical cancer is largely preventable by immunization and screening. Many kinds of HPV can be prevented from infecting the cervix with vaccination, hence preventing cervical cancer. Screening for cervical cancer can discover precancerous cells in the cervix, which can be treated before they become cancerous.
II. Causes and Risk Factors
Human Papillomavirus (HPV) infection
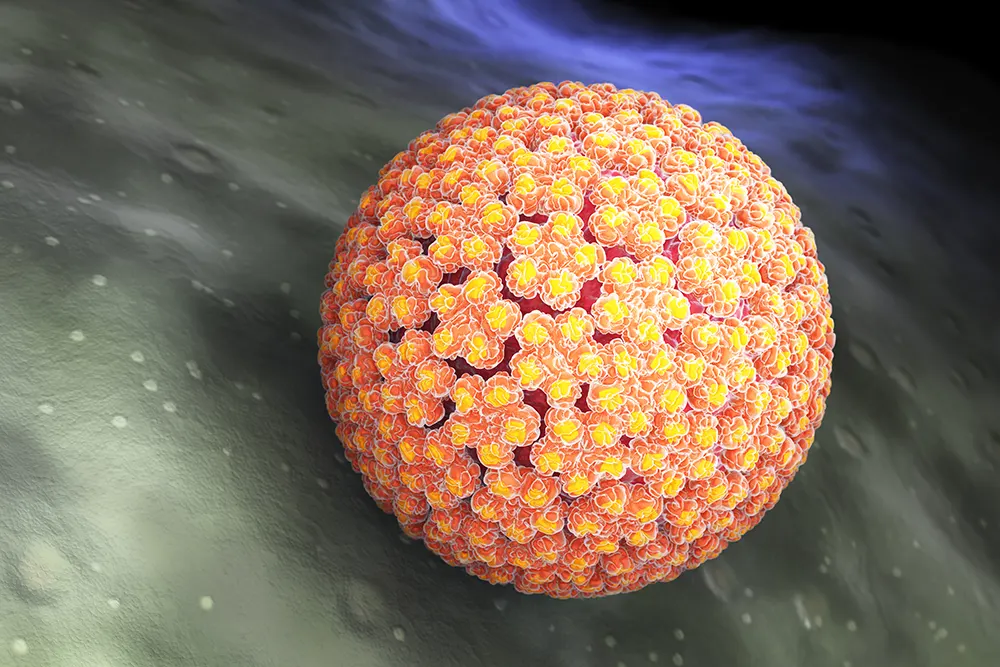
The most frequent reason for cervical cancer is human papillomavirus (HPV). The cervix and other body areas are susceptible to HPV , a group of viruses. Certain HPV strains can alter cervix cells and increase the risk of cervical cancer. Even though there are over 100 different varieties of HPV , only a few of them are known to cause cervical cancer.
Smoking and other lifestyle factors

Another risk factor for cervical cancer is smoking. Cervical cancer in women is twice as likely to occur in smokers as in non-smokers. Additionally , smoking raises the possibility of dying from cervical cancer. The consumption of a diet low in fruits and vegetables, being overweight or obese and long-term use of oral contraceptives are other lifestyle choices that may raise the risk of cervical cancer.
Weak immune system
Women who have compromised immune systems are more likely to get cervical cancer. Women with HIV or AIDS , those who have undergone organ transplantation, and those on immunosuppressant medications are all included in this category.
Family history and genetic predisposition
There may be a higher risk of cervical cancer in women who have a family history of the condition.
Cervical cancer risk can also be increased by inherited genetic disorders like Lynch syndrome. The chance of developing cervical cancer is also higher in women who have inherited specific genetic abnormalities, such as BRCA1 and BRCA2.
In conclusion, a number of things can lead to cervical cancer, including HPV infection, smoking and other lifestyle choices, a weakened immune system, a family history of the disease and genetic predisposition. Women should be aware of their individual risk factors for developing cervical cancer and take precautions to lower that risk, such as receiving an HPV vaccination and scheduling routine cervical cancer tests.
III. Symptoms and Diagnosis
Common symptoms of cervical cancer
Cervical cancer often has no symptoms in its early stages. As cancer grows, common symptoms may include:
- Vaginal bleeding after intercourse, between periods or after menopause
- Pelvic pain or pressure
- Painful urination
- Vaginal discharge that is thick, heavy or discolored
- Pain during intercourse
It’s important to note that these symptoms can also be caused by other conditions , so it’s important to see a healthcare provider if you experience any of them.
Diagnostic tests, including Pap smear and biopsy
A pelvic examination and Pap test are often the first steps in the diagnosis of cervical cancer. A Pap smear is a test that can find unfavorable cervix cells. Additional testing can be required if aberrant cells are discovered. These procedures could include a colposcopy, which looks at the cervix under a special microscope, and a biopsy, which involves taking a small sample of tissue from the cervix for analysis.
Additional tests may be performed to assess cancer’s stage if cervical cancer is found. MRI, PET, and CT scans are a few possible examinations. These imaging techniques can be used to assess the extent of cancer’s spread as well as whether it has affected any neighboring lymph nodes or organs.
IV. Stages of Cervical Cancer
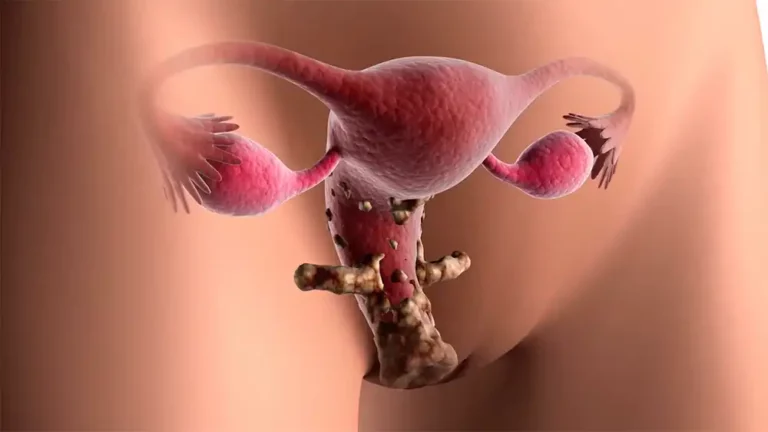
How cervical cancer is staged
Cervical cancer is staged based on the size and spread of cancer. The most commonly used system for staging cervical cancer is the International Federation of Gynecology and Obstetrics (FIGO) system.
The FIGO system has four stages of cervical cancer, numbered 0 through IV.
- Stage 0: Cancer is found only in the surface cells of the cervix.
- Stage I: Cancer is found only in the cervix.
- Stage II: Cancer has spread to the uterus or other nearby structures, but not to the lymph nodes or other parts of the body.
- Stage III: Cancer has spread to the lower part of the vagina and/or the lymph nodes in the pelvis.
- Stage IV: Cancer has spread to other parts of the body, such as the lungs, liver, or bones.
It’s important to note that the stage of cervical cancer can change over time , so a woman may have different treatment options depending on the stage of her cancer at different times.
Importance of staging in determining treatment options
The most effective treatment choices depend on cervical cancer’s stage. Chemotherapy, radiation therapy, or surgery are all possible cervical cancer treatments. The recommended course of therapy will depend on cancer’s stage, the woman’s general health and her personal preferences.
For cervical cancer in its early stages, surgery is frequently the main treatment. A hysterectomy, which involves the removal of the uterus, or a trachelectomy, which involves the removal of the cervix, are examples of surgical procedures. For cervical cancer that has progressed beyond the surgical stage, radiation therapy and/or chemotherapy may be advised in addition to surgery.
Given that cervical cancer is frequently very curable when discovered early, routine screenings and early identification are crucial for enhancing the prognosis for women who develop the disease.
V. Hysterectomy as a Treatment Option
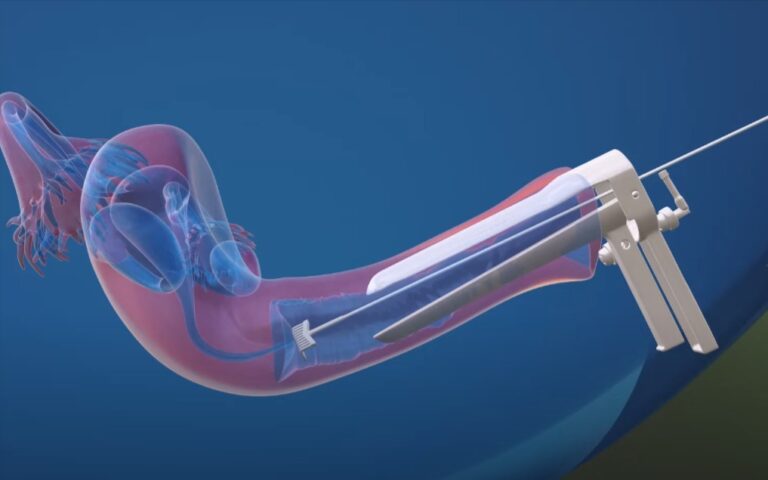
How hysterectomy is used to treat cervical cancer
During a hysterectomy, which is a surgical surgery , the uterus is removed. Particularly while the condition is still in its early stages, it is frequently utilized to treat cervical cancer. When a woman develops cervical cancer, a hysterectomy is performed to remove the malignant tissue and stop the cancer from spreading.
Types of hysterectomy (total, radical, and simple)
There are several types of hysterectomy that can be used to treat cervical cancer. These include:
- Total hysterectomy: This procedure involves the removal of the uterus and the cervix.
- Radical hysterectomy: This procedure involves the removal of the uterus, cervix, and the top portion of the vagina. Additionally , the lymph nodes in the pelvis may also be removed.
- Simple hysterectomy: This procedure involves the removal of the uterus but leaves the cervix in place.
Pros and cons of hysterectomy as a treatment option
In the early stages of the disease, hysterectomy is a very successful cervical cancer therapy option. Hysterectomy does, however , carry certain possible dangers and adverse effects, just like any surgical operation.
Some benefits of hysterectomy include:
- The cancerous tissue is removed, which helps to prevent cancer from spreading.
- It is a highly effective treatment option for early-stage cervical cancer.
- It can be performed through minimally invasive techniques , such as laparoscopic surgery, which can result in less pain and a shorter recovery period.
Some potential risks and side effects of hysterectomy include:
- Any surgical procedure carries the risk of bleeding, infection and other complications.
- Hysterectomy can cause emotional and psychological distress, particularly for women who wish to have children in the future.
- Hysterectomy can cause menopausal symptoms, including hot flashes and vaginal dryness.
How the stage and grade of the cancer influence treatment choice
The stage and grade of cervical cancer play a significant role in determining the best treatment options. For early-stage cervical cancer, hysterectomy is often the primary treatment option. However, for more advanced stages of cervical cancer, radiation therapy and/or chemotherapy may be recommended in addition to surgery.
In addition, the grade of cervical cancer can also influence treatment choice. For cervical cancer that is of a higher grade, more aggressive treatment may be recommended. This may include a radical hysterectomy, which removes the uterus, cervix, and top portion of the vagina, as well as nearby lymph nodes.
VI. Additional Treatment options
Surgery (conization, trachelectomy)
Other surgical procedures are available to treat cervical cancer than hysterectomy. These comprise:
Conization: This technique entails removing a cone-shaped portion of cervical tissue. Cervical cancer is frequently diagnosed with it or at an early stage.
Trachelectomy: This procedure involves the removal of the cervix and the upper part of the vagina , but leaves the uterus in place. It is typically used for women who wish to have children in the future.
Radiotherapy

Radiotherapy, also known as radiation therapy, uses high-energy radiation to kill cancer cells. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy). Radiotherapy is typically used in combination with surgery , particularly for more advanced stages of cervical cancer.
Chemotherapy

Chemotherapy kills cancer cells using medicines. It can be administered intravenously or orally. Typically , chemotherapy is administered in conjunction with surgery, especially for late stages of cervical cancer.
Combination of treatments
Combination therapies may be suggested for cervical cancer in more advanced stages. This could involve radiotherapy, surgery or chemotherapy. The particular course of treatment will depend on cancer’s stage and grade , as well as the patient’s general health and preferences.
VII. Recovery and Follow-up Care
Recovery time and potential complications
The length of recovery following a hysterectomy or other cervical cancer treatment can vary based on the procedure and the patient’s general condition. In general, recovery from a total or radical hysterectomy can last up to 6-8 weeks, although it might take less time for a basic hysterectomy. Physical therapy may be a part of the healing process to aid in the regaining of strength and mobility.
After a hysterectomy, bleeding, infections, blood clots, and anesthesia-related responses are all possible side effects. Following surgery, some women may also experience emotional and psychological problems, including sadness, anxiety and dysfunctional sexuality. It is crucial to seek support from friends, family, and medical experts because these are common reactions.
Importance of follow-up care and monitoring for recurrence
Cervical cancer is a dangerous disorder that needs to be closely watched for recurrence. Regular check-ups with a gynecologist or oncologist as well as imaging tests like CT scans and PET scans to look for any symptoms of recurrence are often part of follow-up therapy.
Follow-up care must be carefully monitored and any new symptoms or changes should be immediately reported to your doctor. With the use of this follow-up care, any potential recurrences may be discovered early and treated more successfully.
VIII. Conclusion
A. The Value of Early Cervical Cancer Detection and Treatment
A woman’s health and well-being may be significantly impacted by cervical cancer, a dangerous disorder. For the greatest results, cervical cancer must be identified and treated as early as feasible. Cervical cancer can be found early on, when it is most curable , by routine screenings like Pap smears and HPV tests.
B. The Treatment of Cervical Cancer with Hysterectomy
Hysterectomy is a surgical surgery that removes the uterus and is utilized as a cervical cancer treatment option. It is often advised for cervical cancer in its advanced stages and is a very powerful therapy option.
C. The Presence of a Variety of Treatment Options
Surgery, radiation, chemotherapy, and a combination of treatments are all available as cervical cancer treatments. The stage and grade of cancer, the patient’s general health, and their personal preferences will all impact the optimal course of treatment for each individual.
D. Working with a Medical Professional
To choose the appropriate course of therapy for the patient, it is crucial to consult carefully with a healthcare practitioner. The finest treatment and assistance can be given by a group of doctors, including gynecologists, oncologists and radiation therapists.
Finally, it is important to emphasize that cervical cancer is a dangerous disease that benefits from early detection and treatment. While there are numerous treatment choices available , including hysterectomy, it is critical to speak with a medical expert to determine which one is best for the patient. Regular screenings and follow-up care help assure the best possible outcome.