5 Years After Hysterectomy: Long-Term Effects and Considerations

Hysterectomy, a frequently performed gynecological procedure for uterine removal, carries significant importance for women’s health. As women progress beyond the 5-year milestone post-hysterectomy, it becomes crucial to explore the potential long-term effects and considerations associated with this surgery. This article aims to delve into various facets of hysterectomy, encompassing its impact on hormonal equilibrium, sexual function, and overall well-being. Furthermore, we will examine the outcomes of endometrial ablation, a procedure occasionally performed concurrently with hysterectomy. Let us now uncover the occurrences in the years following a hysterectomy, along with key awareness for women.
Hysterectomy and Its Consequences
Understanding Hysterectomy
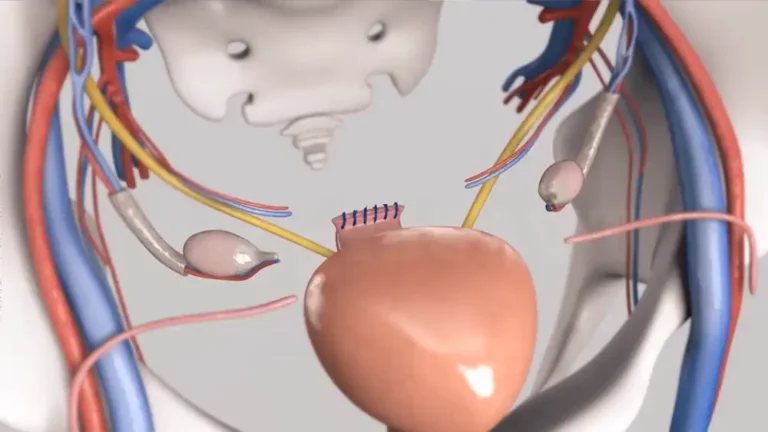
Hysterectomy, a surgical intervention, encompasses the removal of the uterus, and depending on the specific case, it may also involve the extraction of the ovaries, fallopian tubes, and cervix. This surgical procedure offers different approaches, including vaginal, abdominal or laparoscopic methods. Women may opt for hysterectomy to address a multitude of reasons, such as dysfunctional uterine bleeding, fibroids, endometriosis, or other conditions that impact the uterus. It is vital to comprehend the diverse facets of this surgical intervention and its implications thoroughly.
Surgical Menopause and Hormone Replacement Therapy(HRT)
After undergoing a hysterectomy, there can be imbalances in hormone production and equilibrium. If the surgery involves the removal of the ovaries, it can result in surgical menopause, which triggers a sudden decline in estrogen levels. Hormone replacement therapy (HRT) may be considered as a solution to relieve symptoms such as hot flashes, mood swings and vaginal dryness. However, it is crucial to consult with a healthcare professional before making a decision about using HRT, taking into account the person’s unique health factors and requirements.

Impact on Sexual Function
Hysterectomy can potentially influence sexual function and intimacy. Some women report changes in sexual desire, arousal, or orgasmic response after the procedure. Vaginal dryness, reduced lubrication, and discomfort during intercourse may also occur. Open communication with one’s partner and healthcare provider is crucial in addressing these concerns and exploring potential solutions.
Considerations for Uterine and Ovarian Health
While hysterectomy effectively resolves conditions affecting the uterus it is essential to consider the implications for long-term uterine and ovarian health. The removal of the uterus eliminates the risk of uterine-related issues, such as uterine cancer or dysfunctional uterine bleeding. However, it does not eliminate the risk of ovarian cancer. Women with intact ovaries should remain vigilant about monitoring their ovarian health and discuss any concerns with their healthcare provider.

Endometrial Ablation for abnormal Uterine bleeding
Exploring Endometrial Ablation
Endometrial ablation is a commonly employed procedure that is frequently carried out alongside a hysterectomy. Its primary purpose is to address dysfunctional uterine bleeding, whereby the endometrial lining of the uterus is removed or destroyed. The objective of this procedure is to diminish or eradicate the occurrence of heavy or prolonged menstrual bleeding, presenting an alternative for women who desire to retain their uterus. Nevertheless, it is crucial to acknowledge that endometrial ablation is not suitable for every individual, and the decision to undergo this procedure should be made following a comprehensive evaluation and consultation with a healthcare professional.
Long-Term Outcomes and Considerations
Women who undergo endometrial ablation should take into account the long-term implications of the procedure. Although it can offer relief from menstrual problems, it does not ensure permanent outcomes. Some women may encounter a reoccurrence of symptoms as time passes. Therefore, it is crucial to engage in a discussion with a healthcare provider regarding the potential advantages, risks, and anticipated results.
Research Insights: Mayo Clinic Cohort Study
Examining Long-Term Effects
The Mayo Clinic conducted a cohort study to investigate the long-term effects of hysterectomy and shed light on the experiences of women who had undergone this procedure. The study aimed to assess factors such as overall health, hormonal changes, and quality of life among women in the 5-year post-hysterectomy period.
The findings of the Mayo Clinic cohort study indicated several important insights. Firstly, it highlighted that women who had a hysterectomy experienced improvements in symptoms related to the conditions that led to the procedure, such as dysfunctional uterine bleeding or fibroids. These improvements were sustained over the 5-year period, indicating the long-lasting benefits of hysterectomy.

Additionally, the study revealed that women who had their ovaries removed during hysterectomy faced a higher risk of entering surgical menopause and experiencing the associated symptoms of low estrogen levels. It emphasized the importance of hormone replacement therapy (HRT) in managing menopausal symptoms and preserving overall well-being.
Another aspect explored in the study was the impact of hysterectomy on cardiovascular health. It suggested that women who had undergone a hysterectomy, especially those with oophorectomy (removal of the ovaries), might be at a slightly higher risk of coronary heart disease. These findings highlight the importance of considering cardiovascular health and adopting preventive measures, such as a healthy lifestyle and regular check-ups, following a hysterectomy.
The Mayo Clinic study also addressed concerns related to sexual function and pelvic health. While some women reported improvements in sexual satisfaction and relief from conditions that may have previously impacted their sex life, others experienced changes in sexual function. Factors such as vaginal dryness and decreased libido were identified as potential challenges that women may face after hysterectomy. The study emphasized the need for open communication with healthcare providers and exploring options for managing these concerns, such as vaginal lubricants or hormone therapy.
It is important to note that every individual’s experience with hysterectomy is unique, and the findings of the cohort study provide valuable insights on a broader scale. The study also acknowledged the limitations of the research, including potential biases and the need for further investigation.
Conclusion: Empowering Informed Decisions 5 Years after Hysterectomy
As women reach the milestone of 5 years following a hysterectomy, it is crucial to consider the potential long-term effects and implications of this procedure. The Mayo Clinic cohort study, along with other research, contributes to our understanding of the post-hysterectomy journey and empowers women to make informed decisions about their health.
If you have undergone a hysterectomy or are contemplating the procedure, it is crucial to engage in open communication with your doctor and have a thorough discussion about your individual circumstances. This conversation should encompass various factors such as hormonal balance, sexual function, and overall well-being. By doing so, your healthcare provider can offer personalized guidance tailored to your specific needs, assisting you in navigating the potential risks and benefits associated with a hysterectomy.
Remember, every woman’s experience is unique, and the decision to undergo a hysterectomy should be based on a thorough evaluation of your individual needs and in consultation with a qualified healthcare professional. By staying informed and proactively addressing any concerns, you can navigate the journey of 5 years after hysterectomy with confidence and optimize your long-term health and well-being.
FAQs
What is the role of the National Health Service (NHS) in hysterectomy procedures?
The NHS provides healthcare services, including hysterectomy procedures, in the United Kingdom. It offers information and guidance on the topic.
How does a hysterectomy affect life expectancy?
Hysterectomy itself does not directly affect life expectancy. However, individual health factors and underlying conditions can influence overall life expectancy.
What is a TCRE or hysterectomy, and how does it compare with less invasive methods?
The abbreviation TCRE stands for transcervical resection of the endometrium. This surgical technique is employed to treat specific conditions of the uterus and is considered less invasive when compared to the conventional hysterectomy procedure.
What are the possible benefits of removing the ovaries during a hysterectomy?
The removal of the ovaries during a hysterectomy can potentially lower the risk of developing ovarian cancer and other related issues affecting the ovaries in the future.
Is there an increased risk of developing postmenopausal complications after a hysterectomy?
Postmenopausal complications can occur after a hysterectomy, but the risk may vary depending on various factors. Discuss with your doctor to understand your specific risks.
How common are subtotal hysterectomies, and what is the difference compared to a total hysterectomy?
Subtotal hysterectomies, where only a portion of the uterus is removed, are less common than total hysterectomies. The main difference is that in a subtotal hysterectomy, the cervix is usually left intact while in a total hysterectomy, both the uterus and cervix are removed.
What is the role of the Department of Health in issues related to hysterectomy?
The Department of Health, in various countries, plays a role in setting guidelines, policies, and regulations related to hysterectomy procedures, ensuring quality care and patient safety.
Can Low Estrogen after a hysterectomy impact a woman’s reproductive system?
Loss of estrogen after a hysterectomy, especially when the ovaries are removed, can lead to changes in the reproductive system, including the onset of menopause and changes in fertility.