A New Era in Women’s Health: Supracervical Laparoscopic Hysterectomy Unveiled
Welcome to our comprehensive guide on supracervical hysterectomy. In this article, we will delve into the details of this surgical procedure and explore its various aspects, including its types, indications, benefits, and potential complications. Whether you’re considering a laparoscopic, abdominal or vaginal hysterectomy, this guide aims to provide you with valuable insights to make informed decisions regarding your health.

Understanding Hysterectomy
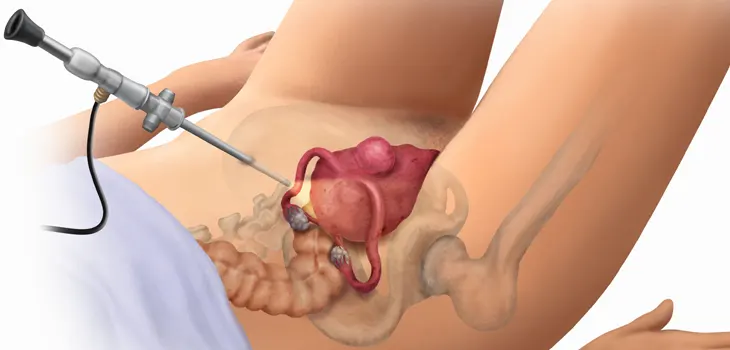
Hysterectomy, a surgical intervention, involves the removal of the uterus and sometimes accompanying reproductive organs like the ovaries and fallopian tubes. Widely performed in gynecology, this procedure effectively addresses a range of conditions such as uterine fibroids, abnormal uterine bleeding, endometriosis, and pelvic organ prolapse.
Types of Hysterectomy
There are different types of hysterectomy procedures, including:
- Total Hysterectomy: In this procedure, the entire uterus, including the cervix, is removed.
- Supracervical Hysterectomy: This type of hysterectomy involves removing the uterus while leaving the cervix intact.
- Radical Hysterectomy: This procedure is typically performed for gynecologic cancers and involves the removal of the uterus, cervix, surrounding tissues, and possibly the upper part of the vagina.
Benefits and Risks of Supracervical Laparoscopic Hysterectomy
Supracervical hysterectomy presents a variety of potential advantages when compared to alternative hysterectomy methods. It has the potential to safeguard sexual function, minimize operative times, and result in a shorter hospital stay and recovery period. However, similar to any surgical procedure, there are inherent risks involved, including the potential for postoperative complications like infection, bleeding, and harm to adjacent organs.
Indications for Supracervical Hysterectomy
Supracervical hysterectomy is often considered as a potential option for treating particular benign gynecologic conditions. This includes cases involving uterine fibroids, abnormal uterine bleeding, and select instances of endometriosis. It is essential to have a consultation with your healthcare provider to assess whether supracervical hysterectomy is the appropriate choice for your specific situation.
Surgical Procedure and Recovery
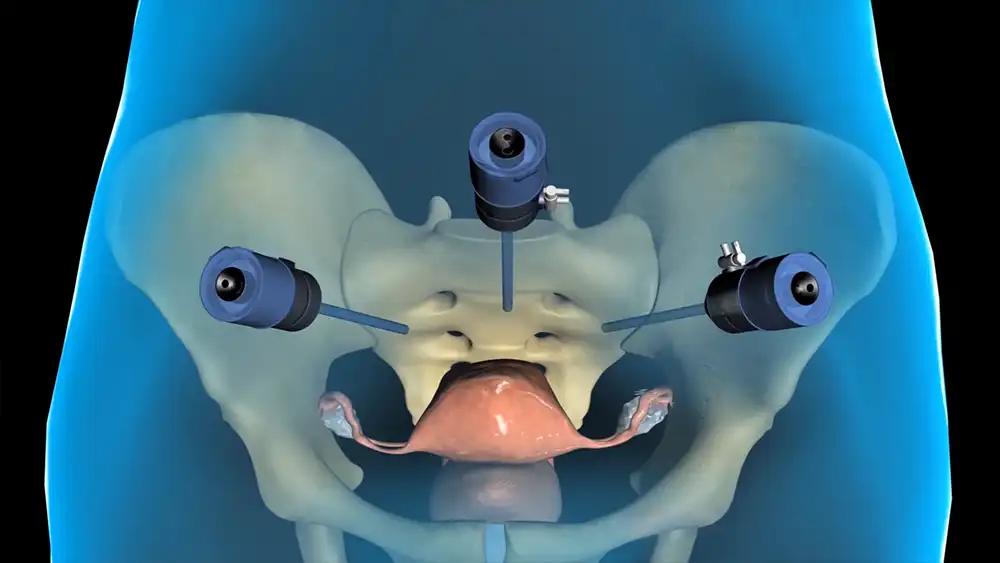
During a supracervical hysterectomy, the surgeon will make an incision in the abdomen to access the uterus. The uterus is then removed while leaving the cervix in place. The procedure can be performed through minimally invasive techniques such as laparoscopy, which involve smaller incisions and faster recovery times compared to traditional abdominal surgery.
The duration of postoperative recovery after a supracervical hysterectomy can vary from person to person, typically spanning from a few weeks to a couple of months to return to normal. To ensure optimal healing, it is crucial to adhere to your doctor’s instructions and allow yourself ample rest. The resumption of normal activities should be approached gradually, with guidance from your healthcare provider.
Potential Complications and Long-Term Effects
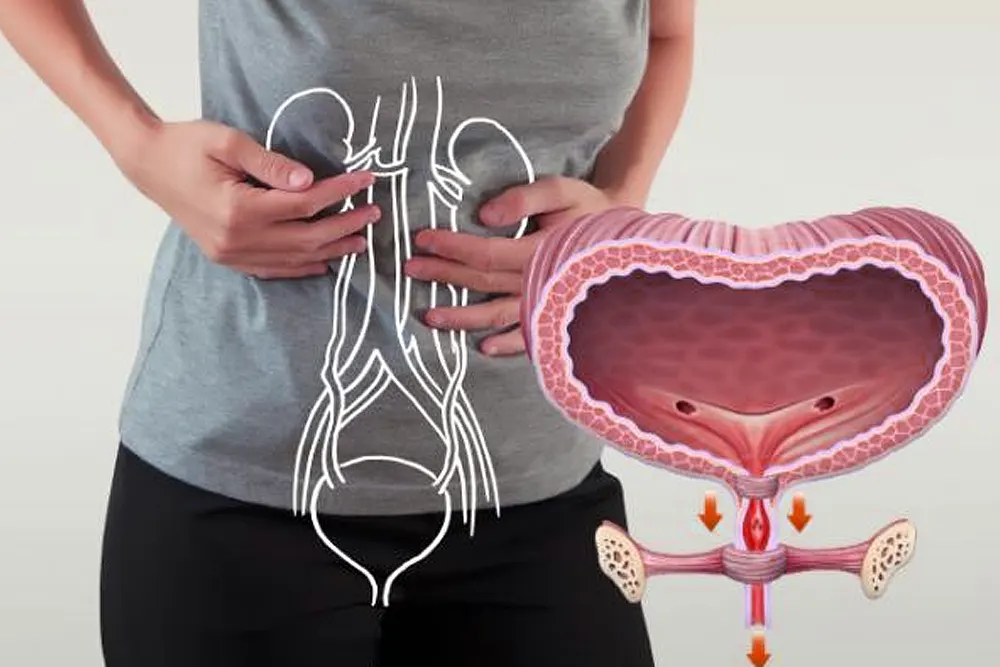
While supracervical hysterectomy is generally a safe procedure, it is not without potential complications. These can include the risk of infection, blood loss, injury to surrounding structures, and urinary or sexual function changes. It is important to discuss these risks with your surgeon before making a decision.
Impact on Hormonal Balance and Sexual Function
Unlike other types of hysterectomy, supracervical hysterectomy does not typically involve the removal of the ovaries, which play a vital role in hormone production. Consequently, immediate menopause is less likely to be induced. However, it’s important to note that natural hormonal changes may still occur gradually, leading to menopause in due course. Consulting with your healthcare provider is crucial to discuss potential impacts on hormonal balance and explore strategies to effectively manage any accompanying symptoms.
Urinary and Sexual Function
In comparison to total hysterectomy, supracervical hysterectomy is typically associated with a reduced risk of urinary incontinence. Additionally, preserving the cervix, which contributes to sexual response, may help maintain sexual function. It’s important to note that individual experiences can vary, and it is crucial to have open and honest conversations with your healthcare provider regarding any concerns or potential changes in sexual function that may arise following the surgery.
Choosing the Route of Hysterectomy
When contemplating a hysterectomy, it is crucial to engage in a thorough discussion with your healthcare provider to determine the most appropriate approach for your individual condition. Several factors, including the size of the uterus, the presence of fibroids or other abnormalities, and your overall health, will be carefully considered. Depending on these factors, options such as laparoscopic, abdominal, or vaginal hysterectomy may be presented to you. Each approach possesses unique advantages and considerations, and your healthcare provider will provide invaluable guidance to assist you in making an informed and personalized decision.
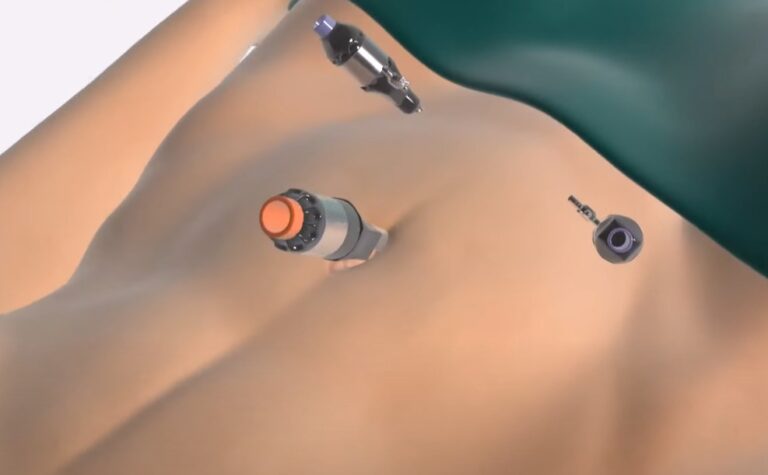
Minimally Invasive Techniques
In recent years, there has been a shift towards minim invasive hysterectomy techniques like laparoscopic surgery or robotic-assisted procedures. They involve smaller incisions, less blood loss, shorter hospital stays, and faster recovery. However, suitability depends on individual circumstances and is determined by the surgeon.
Conclusion
Supracervical hysterectomy is a surgical procedure that offers certain advantages and considerations compared to other types of hysterectomy. It may preserve sexual function, lead to shorter recovery times, and allow for a less invasive approach. However, it is crucial to discuss the benefits, risks, and indications with your healthcare provider to determine if it is the right choice for you. Remember, every individual’s situation is unique, and personalized medical advice is essential in making informed decisions regarding your health.
FAQs
How is a supracervical hysterectomy performed?
During a supracervical hysterectomy, the uterus is removed through small incisions using minimally invasive techniques like laparoscopic or robotic-assisted surgery. The surgeon carefully disconnects the ligaments supporting the uterus, separates it from surrounding structures, and removes it while preserving the cervix.
What is the recovery time after a supracervical hysterectomy?
The duration of recovery differs for every individual, although many patients can anticipate resuming their normal activities within a few weeks. It is of utmost importance to be attuned to your body’s signals, progressively increase your activity levels, and adhere to your physician’s guidance to ensure a smooth and successful recuperation.
Are there any risks or complications associated with a supracervical hysterectomy?
Similar to any surgical intervention, a supracervical hysterectomy carries inherent risks and possible complications. These may encompass infection, bleeding, harm to neighboring organs, and anesthesia-related risks. Nevertheless, these risks are typically minimal and can be mitigated through meticulous surgical techniques and diligent post-operative care.
Can a supracervical hysterectomy affect fertility?
No, a supracervical hysterectomy does not affect fertility since it involves a procedure to remove the uterus while preserving the cervix. However, it’s important to note that other factors, such as the underlying condition being treated or the removal of the fallopian tubes, may impact fertility. Consultation with your healthcare provider is essential to understand the potential effects on fertility.
Can a supracervical hysterectomy be performed with other procedures?
Yes, a supracervical hysterectomy can be performed in combination with other procedures depending on the individual’s specific needs. For example, if there are additional gynecologic issues, such as ovarian cysts or endometriosis, the surgeon may recommend concurrent procedures to address those conditions during the same surgery.
What is the morbidity rate associated with supracervical hysterectomy?
Morbidity regards to the occurrence of complications or adverse events related to a surgical procedure. The morbidity rate for supracervical hysterectomy is generally low, but it can vary depending on factors such as the individual’s overall health, surgical technique and post-operative care.
What is the difference between a total laparoscopic hysterectomy and a total abdominal hysterectomy?
Total laparoscopic hysterectomy and total abdominal hysterectomy are different approaches to removing the uterus. Total laparoscopic hysterectomy involves using a laparoscopic camera and specialized instruments inserted through small incisions, while total abdominal hysterectomy procedure requires a larger length abdominal incision.
What are the indications for a supracervical hysterectomy?
Supracervical hysterectomy may be indicated for various gynecologic conditions, including uterine fibroids, dysfunctional uterine bleeding, or cases where preserving the cervix is preferred overall. Your healthcare provider will evaluate your specific condition to determine the most appropriate treatment option available.