Laparoscopic Hysterectomy for Uterine Myomatosis
Indications for laparoscopic hysterectomy
• Endometriosis
• Abnormal uterine bleeding
• Benign adnexal masses
• Chronic pelvic pain related to adhesions, secondary to pelvic inflammatory disease or previous surgery; pathologies that would usually require abdominal access for hysterectomy
• Stage I endometrial, ovarian and cervical cancer
Classification of laparoscopic hysterectomy according to H. Reich
• Diagnostic laparoscopy with vaginal hysterectomy
• Laparoscopic assisted vaginal hysterectomy (LAVH)
• Laparoscopic hysterectomy
• Total laparoscopic hysterectomy (HLT)
• Supracervical laparoscopic hysterectomy (HLS), includes CASH (classical abdominal semm hysterectomy)
• Vaginal hysterectomy with laparoscopic dome suspension
• Laparoscopic hysterectomy with lymphadenectomy
• Laparoscopic hysterectomy with lymphadenectomy and omentectomy
• Laparoscopic radical hysterectomy with lymphadenectomy
• Hybrids. Finally, a final classification corresponds to hybrids, which can present as anomalies and be found both in the endometrium and in the serosa. They are listed by 2 numbers separated by a dash: the first corresponds to the one closest to the uterine cavity (endometrium); Later, the next number refers to where it is in relation to the serosa.
Table 1 includes the main indications for hysterectomy. Intraoperative complications are: vascular lesions 1% (iliac arteries and veins), intestinal lesions, bladder lesions, urethral lesions, rectovaginal lesions. Among Postoperative complications are: intra-abdominal collection of the vaginal vault (prolapse, dehiscence, abscess, hematoma, granuloma), internal fistula (ureterovaginal, vesicovaginal, rectovaginal fistula).
The contraindications of laparoscopic hysterectomy are:
Severe endometriosis (due to the distortion of the anatomy), severe pelvic inflammatory disease, which leaves a severe adherence compromise as a consequence.
The different approaches are:
Abdominal, vaginal, laparoscopic. Alternatives: Robotics, laparoscopy with a single surgical site (LESS), transluminal endoscopic surgery through natural orifice, hand-assisted laparoscopic surgery.
The different approaches were compared and it was found that laparoscopic hysterectomy is associated with a return to activities –on average– at 13.6 days, less intraoperative bleeding, a decrease in hemoglobin of 0.55 g / dL, a reduction in hospital stay to 2 days , decreased infection of the surgical wound, and its disadvantages, a longer surgical time (20.3 minutes) and a high risk of injury to the urinary tract compared to abdominal hysterectomy.
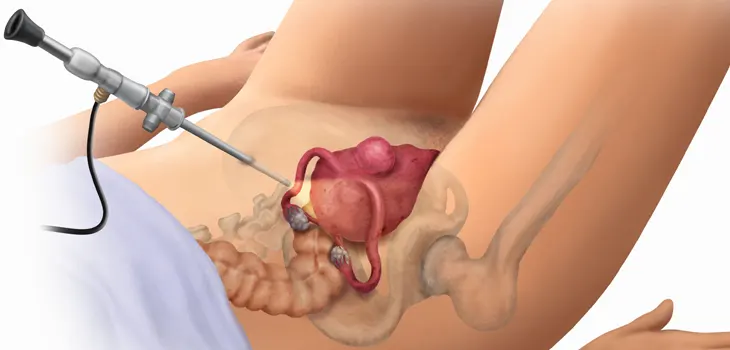
Laparoscopic hysterectomy allows better visualization thanks to the magnification of the existing anatomy and pathology, better access to the fundus of Douglas and the ovarian fossae, better hemostatic control, and avoids abdominal incision pain.
Single-port laparoscopy
Is a variant of laparoscopic hysterectomy. When its advantages were compared in a meta-analysis, no advantages were found over the conventional laparoscopic technique; However, the benefits of the use of a port are more oriented to decisions of an aesthetic nature.
In the current medical literature, no worse results have been reported compared to traditional laparoscopy, and it could be considered when cosmetic care of the patient is desired.
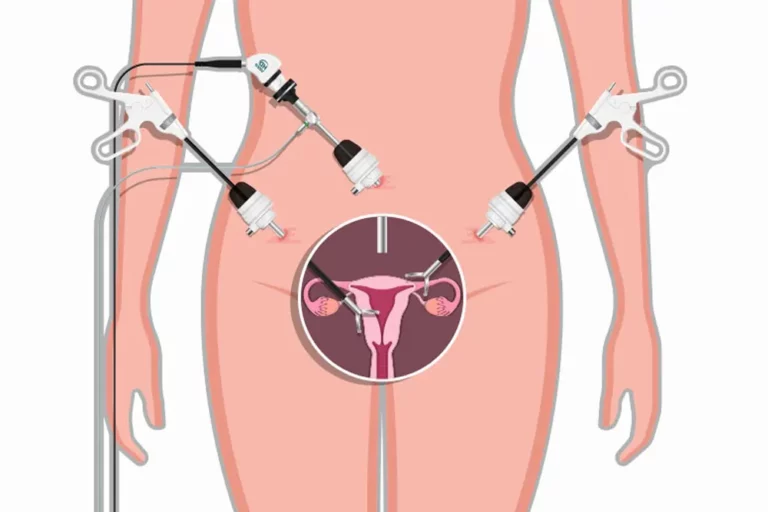
Robotic-assisted hysterectomy
Is a variant of the laparoscopic technique; however, there are still no reports showing that it presents better results than laparoscopy. In addition, it has the disadvantage that it must have previous training, increased cost of equipment and training; and more information on the results of this procedure is still needed. The decision about the access route will depend essentially on the experience and skill of the surgeon.
There are 2 classifications of laparoscopic hysterectomy, one proposed by H. Reich, and the other by Clermont Ferrand:
• Type I. Includes hemostasis and section of the adnexal pedicles and round ligaments, releasing the cusp of the broad ligament and facilitating the rest of the maneuvers vaginally.
• Type II. Associates uterine-vesical detachment and hemostasis of the uterine pedicles.
• Type III. Performs the dissection of the cervix intrafascially, the hemostasis of the cervicovaginal pedicles, and begins the vaginal opening.
• Type IV. It consists of performing the entire hysterectomy laparoscopically, including vaginal opening and closure. The only moment of vaginal use is the extraction of the piece.
The steps to perform a successful laparoscopic total hysterectomy are:
1. Preparation and positioning. The patient is placed in the lithotomy position with both arms bent at the level of the trunk. Keep complete material.
2. Uterine manipulator placement. Before vaginal cleaning, insert a uterine manipulator, although in patients with a very narrow introitus, the uterine manipulator/elevator can be used, and a bladder catheter can be placed with rigorous asepsis.
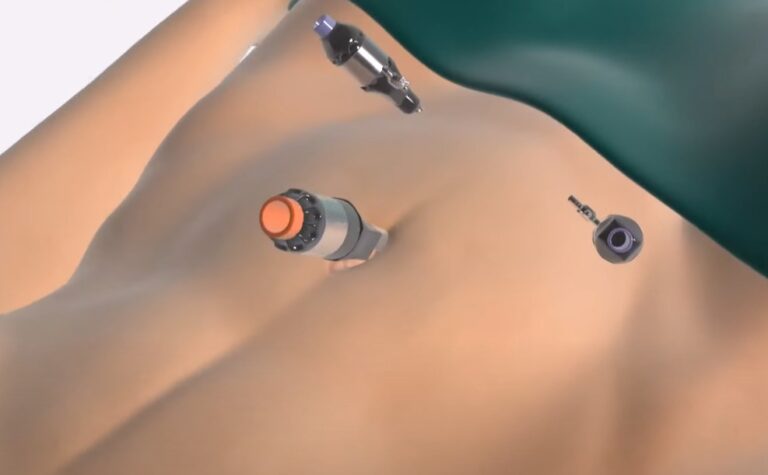
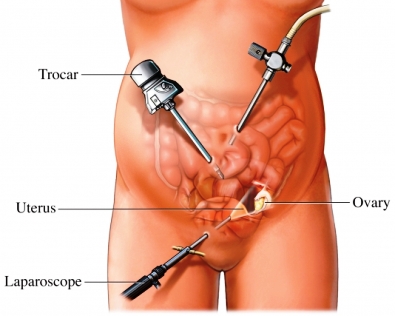
3. Abdominal entry and trocar placement. After placing sterile drapes, the infraumbilical trocar with Veres needle is placed until 15 mmHg intraperitoneal pressure is reached; place the first infraumbilical trocar, and under direct visualization, 2 accessory ports lateral to the rectus abdominis muscles 2 cm below and medially of the anterior superior iliac spine, the right 5 mm and the left 12 mm.
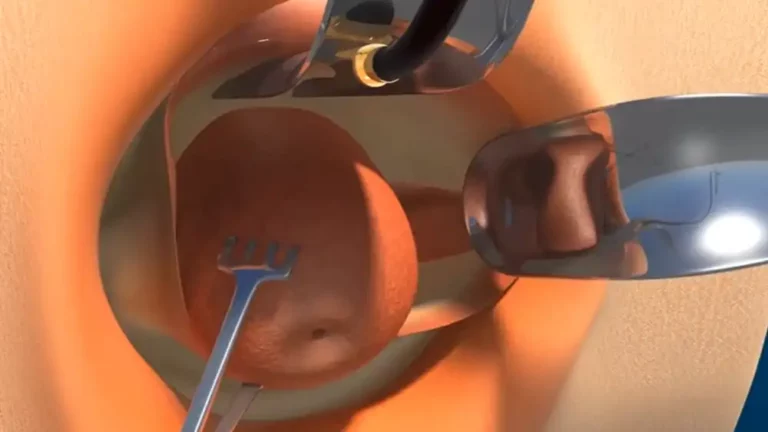
4. Ligation of ovarian vessels. Take and section of round ligament. The infundibulopelvic ligament or utero-ovarian ligament is dissected (depending on the desire for adnexal preservation) with Grasper bipolar versus Harmonic® Scalpel. The uterus is mobilized in a contralateral direction and upwards for better visualization of it.
5. Mobilize the bladder, dissect the broad ligament and separate it into anterior and posterior sheets, moving towards the vesicouterine fold and mobilizing it towards the lower uterine segment (in a patient with a previous cesarean section it may be very elevated) until visualizing the bladder fat, and perform the procedure towards the posterior leaf until cardinal ligament.
6. Ligation of uterine vessels. The uterine artery is skeletonized with a Harmonic scalpel; the vessels are then dissected with bipolar Grasper up to the internal cervical os.
7. Separate the uterus and cervix from the vagina. Identification of the vagina, as well as the internal cervical os with mobilization of the manipulator, perform a cut with a Harmonic scalpel.
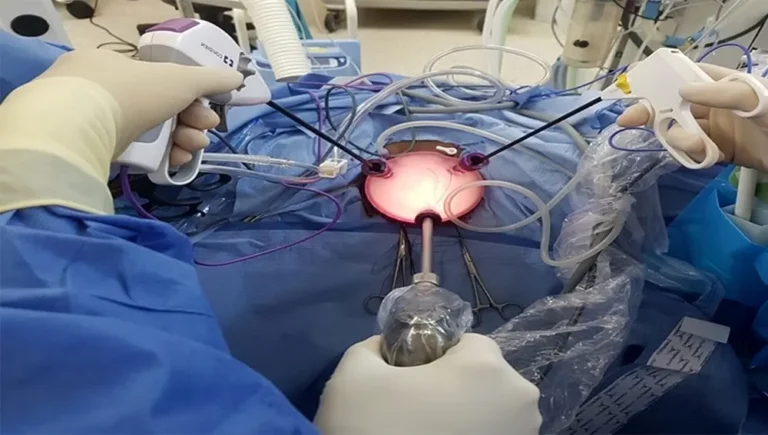
8. Remove the uterus. Place the uterus in the vagina, retaining it to preserve the pneumoperitoneum during suturing. A variant of this step would be the removal of the uterus with a glove and placement of 4 × 4 cm sponges, which can be placed to maintain the pneumoperitoneum; if the uterus is too long to pass through the vagina must be carefully sectioned.
9. Closure of the vaginal vault. We used half of the 14 × 14 cm 0 QuillTM SRS suture. The closure at a distal angle of the vaginal vault is started, ensuring that the rectovaginal fascia, vaginal mucosa and pubocervical fascia are taken, and continue every centimeter of length, cutting the distal end and leaving 12 mm of it; The pelvis is irrigated to verify hemostasis.
10.Closure of ports. Close fascia with 0 vicryl, skin with 4-0 monocryl with continuous subcutaneous stitches.
However, the risk of injury to the urinary tract (bladder or ureter) doubles, and surgical time increases by 30 minutes. Its complications include hemorrhage, dehiscence, fistulas, infection, vessel injury, and bowel injury. The risk of complications after surgery should be explained to patients, since when they feel good, they start physical activities early. Which causes bleeding and pain at the surgical wound site.
There are 2 contraindications to performing laparoscopic hysterectomy:
Significant cardiopulmonary disease with intolerance to increased intraperitoneal pressure, as well as suspicion of malignancy if shredding is required. In public hospitals in our country, it is a little-used practice; However, with current advances, precise indications, and under-experienced hands, the costs of surgical intervention and an early return to work of patients could be considerably reduced. We suggest performing this systematic procedure following the proposals in the literature to safely perform solid organ surgery (hysterectomy).