Ovarian Cyst After Hysterectomy: Understanding the Risks and Management
Introducing our extensive manual on ovarian cysts after hysterectomy. This article provides an in-depth examination of a condition that may develop after undergoing a hysterectomy procedure. We will thoroughly explore the potential risks, symptoms, treatment options, and effective strategies for managing this condition. Whether you have recently undergone a hysterectomy or are contemplating the procedure, it is essential to comprehend the implications of this condition for your overall well-being. Let’s delve into this topic extensively.
What is a Hysterectomy?
Before we delve into ovarian cysts after hysterectomy, it’s essential to understand the basics of a hysterectomy. A hysterectomy is a surgical procedure that involves the removal of the uterus. It may be performed for various reasons, such as managing gynecological conditions like endometriosis, pelvic pain, uterine fibroids, or cancer. The procedure can be performed through different approaches, including abdominal hysterectomy and laparoscopic hysterectomy.
The Connection Between Ovarian Cysts and Hysterectomy
- Overview: Ovarian cysts, fluid-filled sacs forming on or within ovaries, can be categorized as functional or pathological. Functional cysts result from the menstrual cycle, including follicular cysts (when a follicle fails to release an egg) and corpus luteum cysts (when the follicle doesn’t shrink after egg release). Pathological cysts, caused by factors like endometriosis, PCOS, or ovarian tumors, have a small chance of being cancerous. Though they can occur at any age, benign cysts are more common during reproductive years due to hormonal fluctuations and increased follicle development.
- Occurrence of Ovarian Cysts After Hysterectomy Following a hysterectomy, it is still possible to develop this condition, although the incidence is relatively low. In some cases the removal of the uterus during a hysterectomy may affect blood supply or hormonal balance, potentially leading to the formation of benign cysts.
- Symptoms of an Ovarian Cyst This condition can present with a variety of symptoms, including abdominal pain or discomfort, bloating, changes in bowel habits, and pelvic pain. It’s important to note that these symptoms are not exclusive to this condition and may also be attributed to other conditions. Consulting with your healthcare provider is essential for an accurate diagnosis.
- Risks and Complications While most fluid-filled sacs in the ovaries are benign and resolve on their own, some may pose risks and complications. These include the possibility of cyst rupture, torsion (twisting) of the ovary, or the development of malignant (cancerous) cysts. Understanding the potential risks is vital for timely intervention and appropriate management.
Diagnosing and Treating Ovarian Cysts After Hysterectomy
Diagnostic Procedures
The diagnosis of this condition following a hysterectomy typically involves a comprehensive assessment of medical history, pelvic examinations, imaging tests such as ultrasound or MRI, and blood tests to evaluate hormone levels. These diagnostic procedures play a crucial role in determining the characteristics and extent of the cysts.
1. Treatment Approaches
The treatment approach for benign cysts following a hysterectomy depends on several factors, including the size of the cyst, the presence of symptoms, and the overall health of the patient. Available options may include:
- Observation: Small cysts that are asymptomatic can be closely monitored over time to ensure they do not lead to complications.
- Medications: Hormonal therapies, such as birth control pills or hormone replacement therapy, may be prescribed to regulate hormonal imbalances and prevent the formation of new cysts.
- Surgical Intervention: If the cysts are large, causing significant symptoms, or suspected to be cancerous, surgical removal may be necessary.
2. Laparoscopic Approach for Ovarian Cystectomy
Laparoscopic surgery is the preferred method for ovarian cystectomy. Small incisions in the abdomen allow the insertion of a laparoscope and surgical instruments. The laparoscope provides a magnified view, enabling careful cyst removal with minimal damage to surrounding tissues. Benefits include less pain, faster recovery, and better cosmetic outcomes. However, suitability depends on factors like cyst size and patient health.
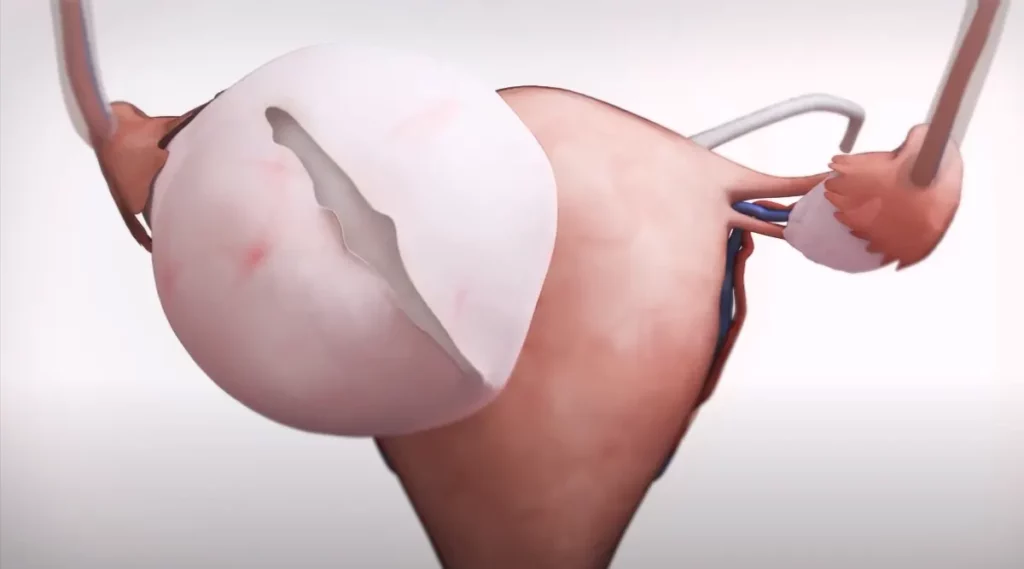
3. Potential Benefits of Laparoscopic Ovarian Cystectomy
Laparoscopic ovarian cystectomy offers several advantages over traditional open surgery. These benefits include:
- Faster Recovery: Due to the smaller incisions, patients often experience less postoperative pain and a quicker recovery time compared to abdominal surgery.
- Reduced Scarring: The smaller incisions result in minimal scarring, promoting better cosmetic outcomes.
- Shorter Hospital Stay: Laparoscopic procedures typically require a shorter hospital stay, allowing patients to return to their daily activities sooner.
4. Monitoring and Follow-Up Care
Following an ovarian cystectomy, it is highly important to prioritize attending regular follow-up appointments with your healthcare provider. These postoperative visits play a vital role in ensuring the ongoing success of your recovery journey. During these appointments, your healthcare provider will carefully monitor your progress, assess any potential complications, and address any postoperative symptoms or concerns you may have.
5. Prevention and Lifestyle Considerations
When it comes to preventing cysts formation after undergoing a hysterectomy, achieving complete prevention may not be guaranteed. However, there are specific lifestyle factors that warrant your attention as they contribute to your overall well-being. By seamlessly integrating these practices into your daily routine, you can proactively work towards maintaining optimal health.
- Maintaining a Healthy Weight: Taking steps to maintain a healthy weight is important for reducing the risk of fluid-filled sacs in the ovaries. Excess body weight has been associated with an increased likelihood of developing cysts. To promote a healthy weight prioritize a balanced diet and engage in regular exercise.
- Hormonal Balance: To maintain hormonal balance and decrease the risk of cyst formation, consult with your healthcare provider about potential hormonal therapies, such as hormone replacement therapy. These therapies can help regulate hormone levels and minimize the chances of cyst development. Your healthcare provider will guide you in determining if hormonal treatments are suitable for your specific needs.
- Regular Pelvic Examinations: Regular pelvic examinations are crucial for monitoring the health of your reproductive organs. Follow your doctor’s recommendations regarding the frequency of these examinations. By attending routine pelvic exams, any potential issues or changes can be detected early, allowing for timely intervention and appropriate management.
Conclusion
In conclusion, while the occurrence of ovarian cysts after a hysterectomy is possible, it is relatively uncommon. However, it is important to be aware of the potential risks, symptoms and treatment options associated with these cysts. If you experience any symptoms or concerns consult with your healthcare provider for proper evaluation and management.
Remember, early detection and timely intervention can significantly reduce the complications associated with this condition. Stay proactive about your health, attend regular check-ups, and maintain open communication with your healthcare team. By doing so, you can take charge of your well-being and ensure a smooth post-hysterectomy journey.
FAQs:
Are ovarian cysts linked to ovarian cancer?
While most fluid-filled sacs in the ovaries are benign and not associated with cancer, there is a potential risk of ovarian cancer development. It is crucial to monitor any suspicious symptoms or changes in the cyst, such as rapid growth or irregularities. Regular follow-up appointments and proper evaluation by a gynecologic specialist can help identify any potential concerns and ensure timely diagnosis and treatment.
What are the risk factors for developing fluid-filled sacs in the ovaries after a hysterectomy?
Several factors can increase the risk of developing fluid-filled sacs in the ovaries after a hysterectomy. These include a history of prior surgeries in the pelvic area, the presence of endometriosis, and retaining one or both ovaries during the hysterectomy procedure. It is essential to discuss these risk factors with your gynecologist to determine appropriate monitoring and preventive measures.
What are the risk factors for developing ovarian cysts after a hysterectomy?
Several risk factors can contribute to the development of ovarian cysts after a hysterectomy. These may include a history of previous surgeries, the presence of certain gynecologic conditions, such as endometriosis, and retaining one or both ovaries during the hysterectomy procedure.
Can ovarian cysts resolve on their own without treatment?
In some cases, small ovarian cysts may resolve on their own without treatment. However, it is crucial to have regular medical evaluations and monitoring to ensure proper management and detect any potential complications.
Can ovarian cysts still develop during menopause?
Yes, ovarian cysts can still develop during menopause. While the occurrence of cysts tends to decrease with age and menopause, hormonal fluctuations and other factors can still contribute to their formation.
Are there any specific risk factors for developing ovarian cysts after a vaginal hysterectomy?
The risk factors for developing ovarian cysts after a vaginal hysterectomy are similar to other types of hysterectomy procedures. Factors such as previous surgeries, underlying gynecologic conditions, and ovarian conservation play a role in determining the risk.
Is it possible to develop ovarian cancer even with intact ovaries after a hysterectomy?
Although the removal of the uterus reduces the risk of ovarian cancer, it is still possible to develop the disease even with intact ovaries after a hysterectomy. Regular medical check-ups and monitoring are essential for early detection and appropriate management