From Incision to Recovery: A Step-by-Step Guide to Vaginal Hysterectomy
I. Introduction
Vaginal hysterectomy is a type of surgery that involves removing the uterus through the vagina. It’s a relatively common procedure that has been around for over a century. In fact, the first vaginal hysterectomy was performed way back in 1853! Over the years the technique has evolved, and now it’s considered a safe and effective option for many women.
According to statistics, vaginal hysterectomy is the preferred approach for about 20% of all hysterectomies performed in the United States.

II. Indications and Preparation
Uterine prolapse, fibroids and unusual uterine hemorrhage are only a few causes for vaginal hysterectomy. Uterine prolapse occurs when the uterus sags and enters the vaginal canal. Fibroids are benign tumors that develop on the uterus and can result in painful periods, pressure in the pelvis, and heavy bleeding. Bleeding that happens in between each menstrual period or after menopause is referred to as abnormal uterine bleeding.
Before the treatment, the patient will have a comprehensive examination to ensure they are in sufficient health to undergo surgery. A physical examination, blood tests and imaging tests like an MRI or ultrasound may all be part of this evaluation.
III. The Procedure: Steps and Surgery Techniques
Anesthesia and positioning of the patient
There are several options for a vaginal hysterectomy, including general anesthesia, spinal anesthesia and epidural anesthesia. General anesthesia keeps the patient completely asleep. Contrary to epidural anesthesia, which requires inserting a catheter into the epidural space to deliver a drug to numb the lower half of the body, spinal anesthesia entails injecting a drug into the spinal canal to achieve the same result.
Once the anesthesia has taken effect, the patient will be placed in the lithotomy position, which consists of lying on one’s back with one’s legs raised and supported in stirrups. The surgeon can easily access the uterus and vagina in this position to execute the operation.
The different techniques
There are numerous ways to carry out the treatment each with advantages and drawbacks of their own.
Total Hysterectomy
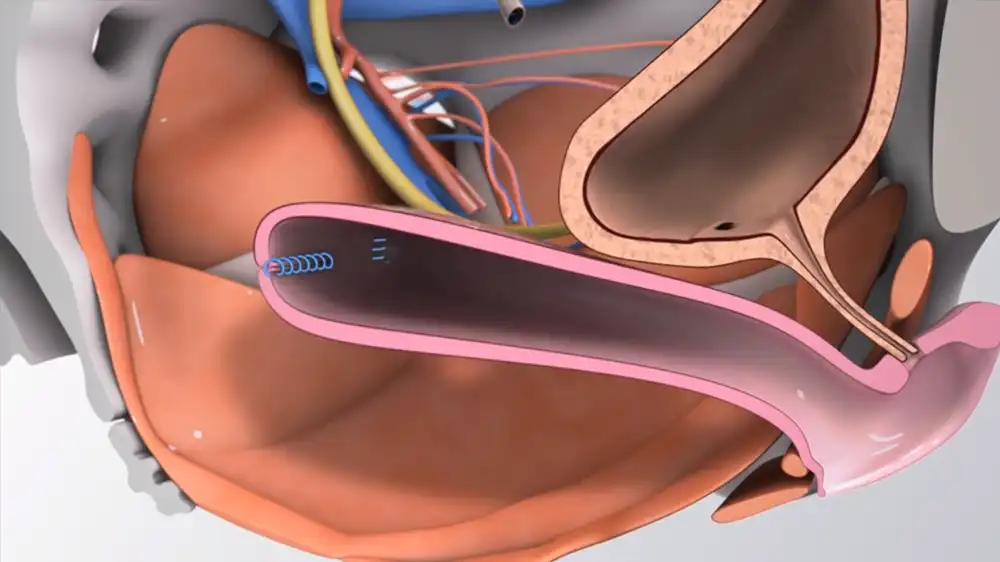
The most widely used method is Total Vaginal Hysterectomy (TVH). Through the vagina, the entire uterus is removed. The uterus will be separated from the surrounding tissues during the process by the surgeon, who will create an incision in the top of the vagina. The uterus is pushed through the vagina and removed when it has been separated.
Because TVH is less intrusive and requires a quicker recovery than other methods, like abdominal hysterectomy (that requires a big abdominal incision), it is frequently chosen over others. But not all patients may be good candidates for TVH, particularly those with significant pelvic adhesions or a history of pelvic surgery.
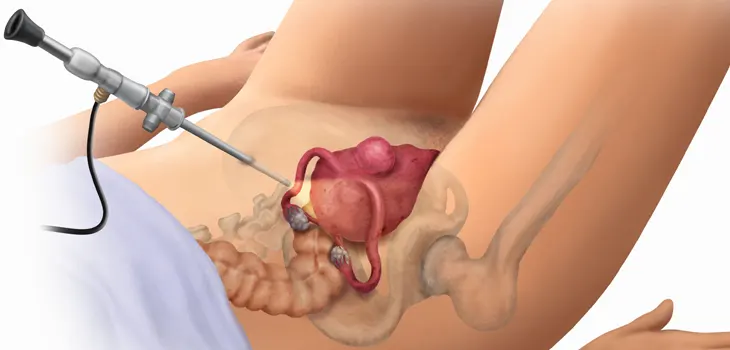
Laparoscopic Hysterectomy
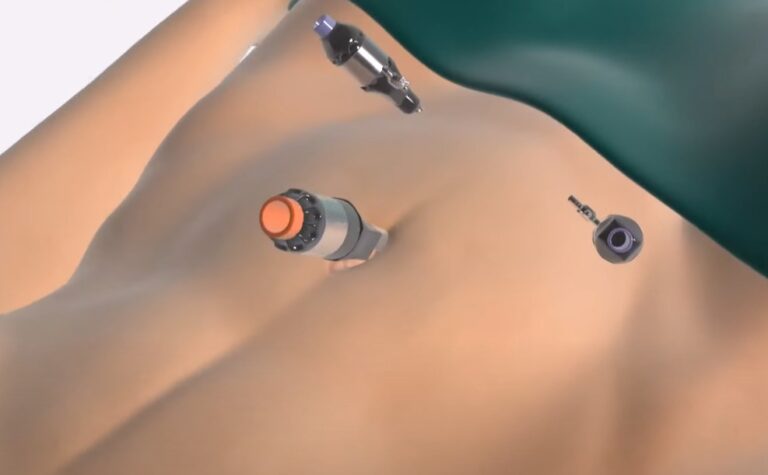
A minimally invasive surgical procedure known as a Laparoscopic-Assisted Vaginal Hysterectomy (LAVH) combines a vaginal approach with the use of laparoscopic tools (Vaginal and Laparoscopic hysterectomy). A laparoscope, which is a short tube with a camera at one end, will be inserted during the treatment through tiny incisions made in the belly.
Similar to TVH, the uterus is separated from the surrounding tissues and dragged into the vagina. LAVH is frequently favored for patients who have undergone pelvic surgery previously or who have extensive pelvic adhesions.
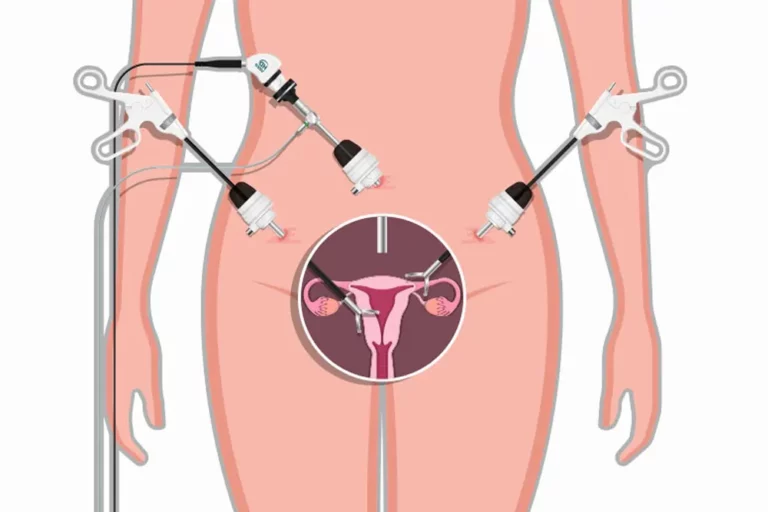
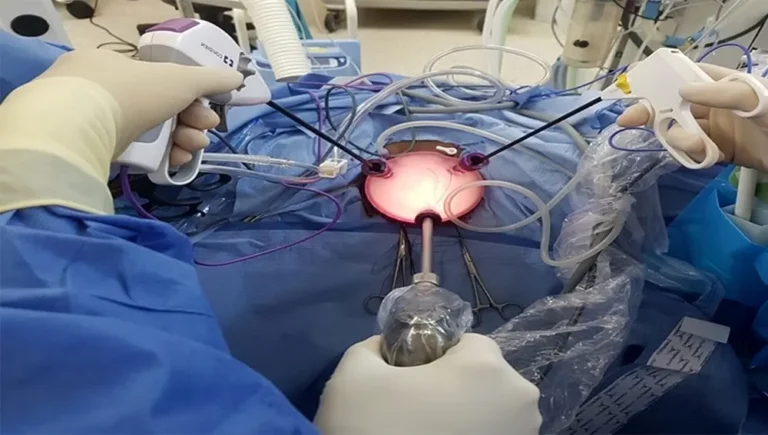
Robotic-Assisted Hysterectomy
A more recent approach called Robotic-Assisted Vaginal Hysterectomy (RAVH) employs robotic technology to carry out the operation. The surgeon operates robotic arms that are holding cameras and surgical equipment during the process. In comparison with an abdominal hysterectomy, only a few small abdominal incisions are used to implant the tools and camera. This technique falls into the category of Laparoscopic hysterectomies.
The uterus is separated from the surrounding tissues using robotic arms that the surgeon controls while looking inside the abdomen. After that, the uterus is taken out via the vagina.
Step-by-step guide on the procedure for Total, Partial, and Radical Vaginal Hysterectomy
Total Hysterectomy:
Pre-operative evaluation
You will go through a complete pre-operative evaluation to determine your suitability for the operation and to evaluate your general health before the procedure. Your doctor will examine you physically, go over your medical history, and prescribe any necessary diagnostic tests such as blood tests.
Anesthesia
You’ll be given anesthetic before the procedure to make you sleepy and block out the pain. Your physician might suggest either a general or regional anesthetic, depending on your particular requirements and choices. You could also have a urinary catheter inserted.
Incision
Your doctor will start the operation by making a little incision in the vagina. The uterus and other reproductive organs can be reached through this incision by the surgeon.
Separation of the uterus
The surgeon will carefully cut apart the uterus from the ligaments, blood arteries, and connective tissues that surround it using surgical instruments. To reduce bleeding, the uterus will be separated from the cervix, and the blood veins that nourish it will be shut.

Removal of the uterus
The surgeon will delicately remove the uterus through the vaginal opening once it has been thoroughly separated. Depending on the operation’s purpose and your particular medical requirements, the ovaries (to avoid the risk of ovarian cancer) and fallopian tubes and lymph nodes may also be removed. Without the need for an external incision.
Closure
The surgeon will carefully use dissolvable stitches to close the vaginal incision once the uterus has been removed. You will be instructed to refrain from sexual activity and vigorous physical activity for a few weeks following the procedure.
Partial Hysterectomy (subtotal Hysterectomy) :
The steps are the same as a total vaginal hysterectomy, however just the portion of the uterus that is impacted by the disorder will be removed by the surgeon. This type of surgery is also known as supracervical hysterectomy.
Radical Hysterectomy:
In a radical vaginal hysterectomy, the ovaries and fallopian tubes may be removed in addition to the uterus, cervix, upper section of the vagina, and tissue around these organs. Women who have been diagnosed with gynecological cancer that has spread beyond of the uterus, cervix, or vagina often receive this recommendation.
A bilateral salpingo-oophorectomy is the surgical elimination of the ovaries and fallopian tubes. Typically, this procedure is performed to reduce the possibility of malignancy recurring or spreading to the ovaries or fallopian tubes. If a woman desires children after surgery, she may contemplate freezing her eggs or using a surrogate.
IV. Recovery and Postoperative Care
Hospital stay and monitoring
The medical staff will monitor your vital signs, such as blood pressure, pulse, temperature and may recommend specific pain management techniques. You may also be given medication to prevent any blood clot and to manage any post operative pain.
During your hospital stay, you’ll be monitored for any signs of complications, such as excessive bleeding or infection. You must follow your doctor’s instructions carefully on how to care for yourself once you leave the hospital. This may include information on how to change your dressings, what to do if you experience any symptoms of infection or complication.
Pain management
Medications
Pain medicines are typically prescribed following surgery. NSAIDs like ibuprofen and naproxen are effective pain relievers. In addition, opioids such as codeine and morphine can be prescribed for more severe pain.
Physical therapy
Following hysterectomy, physical therapy can help mitigate pain and promote healing. Your therapist can direct you through exercises that can improve your circulation, reduce edema, and increase your flexibility.
Heat therapy
Applying heat to the lower abdomen can also help to alleviate postoperative discomfort. A warm compress or heating cloth can be used to increase blood circulation and alleviate pain.
Relaxation techniques
Deep breathing, meditation, and yoga are effective techniques for reducing tension and managing pain. These techniques can aid in promoting flexibility and relaxation.
Dietary changes
Certain nutrients can help to reduce inflammation and promote healing through dietary modifications. Incorporating anti-inflammatory foods into your normal diet, such as turmeric, ginger and verdant greens, can aid in pain management and recovery.
Physical activities and restrictions
Walking
Walking is a crucial activity after surgery. Not only does it promote circulation, but it can also help to prevent blood clots from forming and normalize your bowel movements.
Lifting
It’s important to avoid lifting anything heavier than 10 pounds for at least six weeks after your surgery. This includes activities such as lifting your children or carrying groceries.
Sexual function
You must wait at least six weeks after a surgery before having sexual intercourse. You might have light vaginal bleeding, pain, discomfort, or vaginal dryness during this period.
Exercise
Exercise is crucial for overall health, and bowel movements, but after a vaginal hysterectomy, you should ease into it and gradually increase your training intensity. For six weeks following surgery, refrain from strenuous exercise, such as jogging, weightlifting, and contact sports.
Driving
It’s important to avoid driving for at least two weeks, or until you feel comfortable doing so.
How to take care of the surgical site and prevent infections
It is essential to properly care for the surgical site in order to avoid infection. This includes maintaining a clean and dry environment and avoiding any activities that could introduce microorganisms. This can be accomplished by patting the area with a clean, dry cloth after showering or bathing. I could be needed to wear sanitary pads to absorb any bloody vaginal discharge.
Avoiding heavy lifting and strenuous activity for at least six weeks after surgery is an essential step in preventing infections following the procedure. This will prevent any strain on the surgical site and permit the body to recuperate completely.
As excessive sweating or moisture in the vaginal area can increase the risk of infection, patients should also avoid activities that may cause excessive perspiration or moisture in the vaginal area. Having light vaginal bleeding for some weeks is normal though.
In addition, it is essential to closely monitor the surgical site for signs of infection, such as redness, edema and increased pain.
V. Other treatments
Laparoscopic hysterectomy is a minimally invasive surgical procedure that uses a laparoscope to remove the uterus. The laparoscope is inserted through small incisions in the abdomen and the uterus is removed in small pieces. This procedure has a shorter recovery time compared to abdominal hysterectomy and is associated with less pain and scarring. However, it may not be suitable for all women, particularly those with large fibroids or extensive endometriosis (when endometrial tissue, or similar, grows outside your uterus).
Robotic-assisted hysterectomy is a type of laparoscopic hysterectomy that employs a robotic system to help with the procedure. It has similar techniques, but the surgeon controls robotic arms to perform the surgery.
Abdominal hysterectomy, a traditional surgical technique, involves creating a large incision in the abdomen to take out the uterus. This procedure is usually reserved for women with large uterine fibroids, extensive endometriosis or cancer.
Non-surgical alternatives include medication and hormone replacement therapy. Medications can be utilized to alleviate pain and bleeding caused by uterine fibroids and endometriosis. Hormone therapy can help regulate the menstrual cycle and alleviate severe menopausal symptoms.
Endometrial ablation is another non surgical procedure that is used to treat heavy menstrual bleeding. It involves destroying the lining of the uterus using heat, cold or other methods. This procedure is minimally invasive and has a quick recovery time, but it may not be suitable for women who wish to preserve their fertility.