Tubal Ligation vs Hysterectomy: A Comprehensive Comparison of Sterilization and Risk Factors
Reproductive health offers women various options, including tubal ligation and hysterectomy. Tubal ligation, or “getting one’s tubes tied,” is a permanent sterilization method that blocks the fallopian tubes, preventing fertilization. Hysterectomy involves removing the uterus and is used to treat medical conditions or provide definitive birth control. The decision to undergo these procedures depends on individual factors, and consulting with healthcare professionals is essential. Both procedures carry risks, and tubal ligation is less invasive with a lower risk profile. Hormonal and menstrual changes may occur after a hysterectomy, and there may be an association between these procedures and the risk of ovarian cancer. Further research is needed to understand this relationship fully.

Tubal Ligation: A sterilization procedure Overview
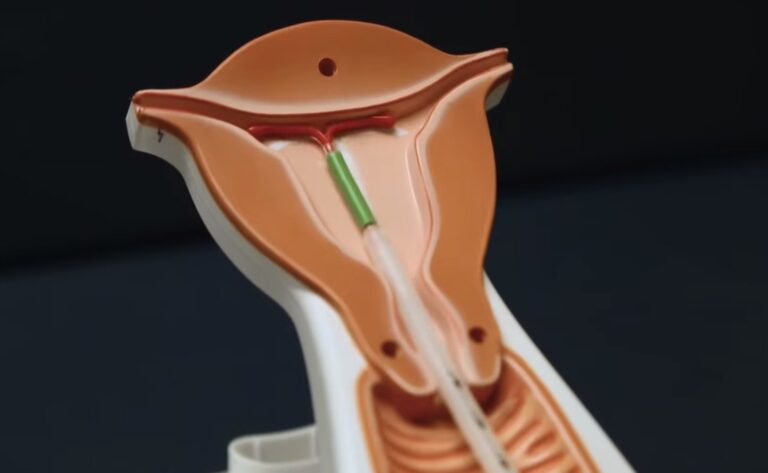
Tubal ligation commonly known as “getting one’s tubes tied,” is a surgical technique mainly used for sterilization. Its main objective is to close or block the fallopian tubes, thus preventing sperm from fertilizing the egg. This procedure provides a permanent means of contraception and is widely recognized as a highly definitive form of birth control.
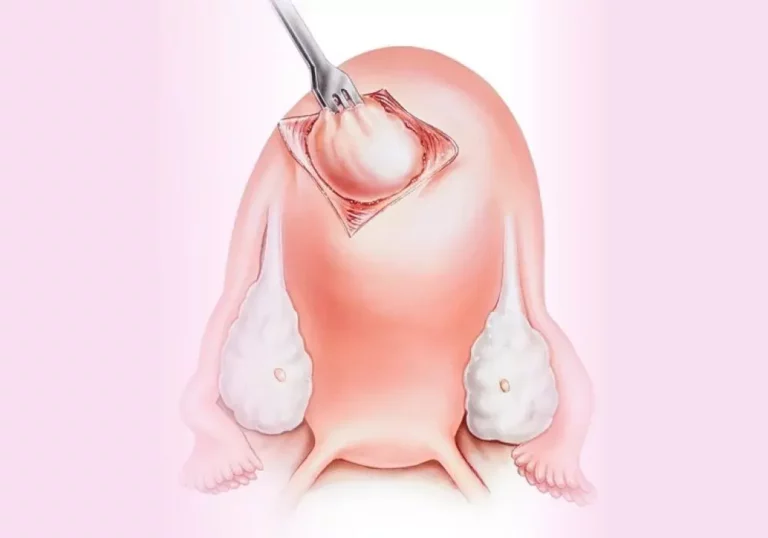
Laparoscopic Tubal Ligation
One common approach to tubal ligation is laparoscopic tubal ligation. This minimally invasive procedure allows for a quicker recovery time and involves making small incisions in the abdomen. The surgeon can access and close off the fallopian tubes through these incisions using various techniques, such as clips, rings, or electrocoagulation.
Risks and Considerations
While tubal ligation is generally considered safe, like any surgical procedure, it carries some risks. These risks include infection, bleeding, damage to surrounding organs, or an adverse reaction to anesthesia. It’s essential to discuss these potential risks with your healthcare provider and understand the implications before proceeding with tubal ligation.
Hysterectomy: A Comprehensive Understanding
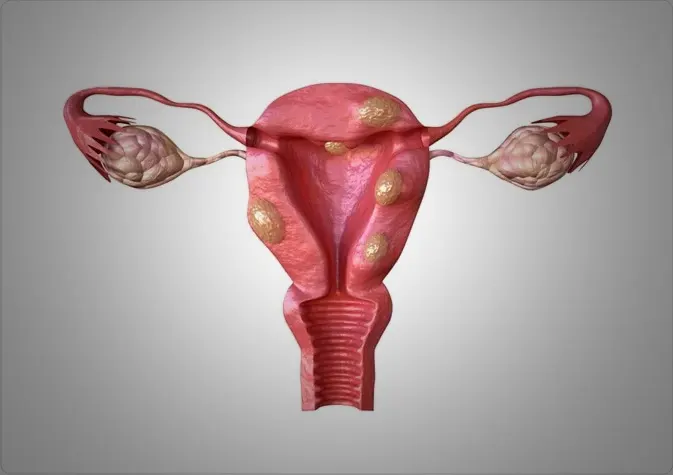
A hysterectomy is a surgical procedure that implies removing the uterus, making it a more comprehensive operation compared to tubal ligation. This surgery is conducted for several purposes, including treating conditions like uterine fibroids, endometriosis, adenomyosis, or certain types of cancer. Furthermore, it can also serve as a permanent form of contraception.
Types of Hysterectomy
The procedures for hysterectomy can vary based on the extent of removal required. There are several common types, including total hysterectomy, which involves removing the uterus and cervix; subtotal hysterectomy, where the uterus is removed while preserving the cervix; and radical hysterectomy, which entails removing the uterus, cervix, and surrounding tissues.
Laparoscopic Hysterectomy
Much like tubal ligation, laparoscopic techniques are frequently employed for hysterectomy procedures. Laparoscopic hysterectomy utilizes small incisions through which a laparoscope and surgical instruments are inserted to remove the uterus. This approach provides advantages such as minimized scarring, shorter hospital stays, and quicker recovery periods.
Risks and Considerations
As with any major surgery, hysterectomy carries potential risks and complications. These may include bleeding, infection, damage to nearby organs, blood clots, or adverse reactions to anesthesia. It’s crucial to have a detailed discussion with your healthcare provider to weigh the risks and benefits based on your specific medical condition.
Comparing tubal sterilization and Hysterectomy
Now that we better understand tubal ligation and hysterectomy, let’s compare these procedures in various aspects.
Sterilization
Both tubal ligation and hysterectomy offer a form of sterilization. Tubal ligation achieves this by blocking or closing the fallopian tubes, while hysterectomy removes the uterus entirely. It’s essential to consider the potential long-term implications and irreversible nature of sterilization before making a decision.
Risks and Complications
Tubal ligation and hysterectomy have distinct risks and potential complications. Tubal ligation, being a less invasive procedure, typically has lower risks in comparison to hysterectomy. The risks associated with tubal ligation include infection, bleeding, and potential harm to neighboring organs. Conversely, hysterectomy involves a more extensive surgical intervention and carries risks such as infection, bleeding, damage to adjacent organs, and blood clots. It is vital to have a thorough discussion about these risks with your healthcare provider in order to make an informed decision.
Impact on Hormone Levels and Menstrual Cycle
Generally, tubal ligation does not directly affect hormone levels or the menstrual cycle. Nonetheless, some women may encounter alterations in their menstrual flow or cycle after the procedure. On the other hand, a hysterectomy involves the complete removal of the uterus, which can lead to the cessation of menstrual periods.
Association with Ovarian Cancer
Research has explored the relationship between tubal ligation, hysterectomy, and the risk of ovarian cancer. Some studies suggest that tubal ligation may be associated with a reduced risk of ovarian cancer, while the removal of both fallopian tubes during hysterectomy further lowers the risk. It’s important to note that these findings are based on observational studies, and individual risks may vary.
Considerations for Future Pregnancy
Both tubal ligation and hysterectomy are considered permanent methods of birth control. Tubal ligation aims to prevent pregnancy by blocking the fallopian tubes, while hysterectomy eliminates the possibility of pregnancy altogether. It’s crucial to carefully consider your future reproductive plans before opting for these procedures, as reversal options may be limited or not possible.
Long-Term Health Considerations
Tubal ligation and hysterectomy may have implications for long-term health. While tubal ligation is generally considered a safe procedure, some studies have suggested a possible association between tubal ligation and an increased risk of certain health conditions, such as cardiovascular disease or menstrual disturbances. Hysterectomy especially if the ovaries are also removed, can have additional effects on hormonal balance and long-term health. It’s important to discuss these potential considerations with your healthcare provider.
Conclusion
Tubal ligation and hysterectomy are two separate procedures with distinct objectives and consequences. Tubal ligation provides a permanent solution for contraception, while a hysterectomy is performed to remove the uterus due to different medical conditions. It is vital to acknowledge that each procedure carries its own risks and factors to consider, which necessitate a thorough consultation with your healthcare provider. Developing an understanding of the disparities between tubal ligation and hysterectomy enables you to make an informed choice regarding your reproductive health and goals for family planning.
FAQs
What is the difference between tubal ligation and hysterectomy?
Tubal ligation is a surgical sterilization procedure that blocks or seals a woman’s fallopian tubes, preventing eggs from reaching the uterus and achieving pregnancy. On the other hand, a hysterectomy is a surgical procedure that involves the removal of the uterus. It is usually performed for various medical reasons unrelated to contraception.
Can tubal ligation be reversed if a woman wishes to become pregnant in the future?
Tubal ligation is broadly recognized as an irreversible method of contraception. Although there exists a procedure known as a tubal reversal, its success cannot be guaranteed in all cases. The result of tubal reversal is influenced by several factors, such as the specific type of tubal ligation initially performed, the remaining length of the fallopian tubes and the extent of cicatricial tissue formation.
Is there a condition known as “tubal ligation syndrome”?
No, “tubal ligation syndrome” is not a recognized medical condition. However, it is important to note that some women may encounter alterations in their menstrual bleeding patterns or experience other symptoms following tubal ligation. These changes are typically unrelated to the procedure itself and may stem from various factors such as hormonal fluctuations or other underlying gynecological conditions. It is advisable for women experiencing such symptoms to consult with their healthcare provider for a thorough evaluation and appropriate management.
Are women who undergo tubal ligation more likely to undergo hysterectomy later in life?
The connection between tubal ligation and the likelihood of a subsequent hysterectomy is not firmly established. Although some studies have indicated a potential association, additional research is required to comprehensively comprehend the relationship between these two procedures and the factors that might influence the necessity of a hysterectomy. Further investigation will contribute to a clearer understanding of the interplay between tubal ligation and the potential need for hysterectomy.