Yeast Infection after Hysterectomy: Understanding Causes, Symptoms, and Vaginal Treatment
Yeast infections are a common concern for many women, and they can occur after undergoing a hysterectomy. In this comprehensive guide, we will explore the connection between hysterectomy and such infections, delve into the causes and symptoms, and discuss various treatment options available. So, if you’ve experienced a vaginal thrush after a hysterectomy or simply want to learn more about it, keep reading!
What is a Hysterectomy?
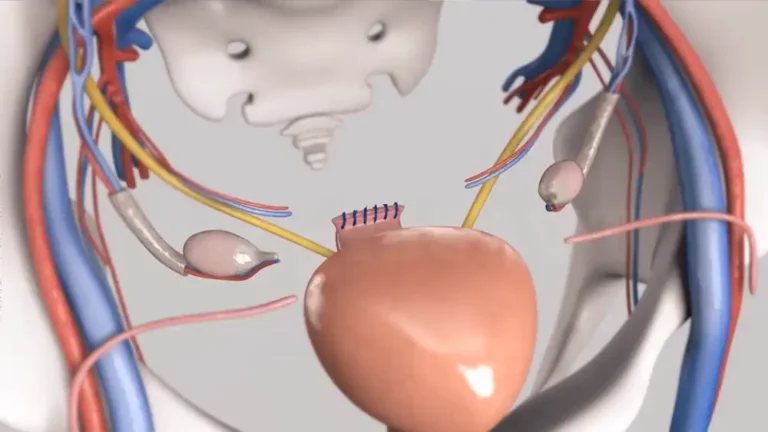
To better comprehend yeast infections after a hysterectomy, let’s begin by gaining a clear understanding of what a hysterectomy involves. A hysterectomy is a surgical procedure that entails the removal of the uterus. It is employed to address various gynecological conditions, such as fibroids, endometriosis, or certain types of cancer.
The Link Between Hysterectomy and Yeast Infections
After undergoing a hysterectomy, some women may experience an increased risk of developing yeast infections. Yeast infections, also known as vaginal candidiasis or vaginitis, occur when there is an overgrowth of Candida albicans, a type of fungus that normally lives in the vagina.

Understanding Yeast Infections
What Causes Yeast Infections?
Yeast infections can have several underlying causes, and certain factors may increase the likelihood of developing them. Let’s take a closer look at some of the key causes and risk factors:
Antibiotics: The use of antibiotics can disrupt the natural balance of bacteria in the vagina, allowing yeast to overgrow.
- Hormonal Changes: Fluctuations in estrogen levels, such as those that occur during menopause or hormone replacement therapy, can create an environment conducive to yeast overgrowth.
- Weakened Immune System: Individuals with compromised immune systems, such as those undergoing oncology treatments, may be more susceptible to yeast infections.
- Tight-Fitting Clothing: Opting for snug or non-breathable attire can create a warm and moist environment, facilitating the growth of yeast.
- Diabetes: Unmanaged diabetes can result in high blood sugar levels, providing a favorable environment for yeast to multiply.
Sexual Activity: Specific sexual practices or the presence of sexually transmitted infections can heighten the likelihood of yeast infection occurrence.
Common Symptoms of Yeast Infections
Yeast infections can cause a range of uncomfortable symptoms, including:
- Itching and irritation in the vaginal area
- Vaginal discharge that is typically thick, white, and odorless
- Redness and swelling of the vulva
- Pain or discomfort during sexual intercourse or urination

It’s important to note that not all yeast infections present with the same symptoms, and some individuals may experience mild or no symptoms at all.
Diagnosis and Treatment Options
If you suspect you have developed a yeast infection after undergoing a hysterectomy or encounter any symptoms related to it, it is vital to seek guidance from a healthcare provider, preferably a gynecologist. They will conduct a comprehensive assessment, which may involve:
- Review your medical history, including details regarding your recent hysterectomy.
- Conducting a physical examination of the vaginal area
- Collecting a vaginal swab for laboratory analysis, often known as a wet mount, to confirm the presence of yeast
Once diagnosed, several treatment options are available to manage yeast infections. These may include:
1. Antifungal Medications: Over-the-counter (OTC) antifungal creams, suppositories, or oral medications, such as fluconazole, can effectively treat yeast infections.
2. Prescription Medications: In some cases, stronger prescription antifungal medications may be necessary, especially for recurrent or more severe infections.
3. Lifestyle and Hygiene Practices: Simple measures like avoiding the use of scented products in the genital area, practicing good hygiene, wearing cotton underwear, and avoiding tight-fitting clothing can help alleviate symptoms and prevent future yeast infections.
4. Addressing Underlying Conditions: In cases of recurring or persistent yeast infections, your healthcare provider may explore potential underlying factors such as hormonal imbalances or immune system issues. Treating these underlying conditions can effectively reduce the likelihood of future infections.
5. Education and Support: Your healthcare provider is a valuable resource for information on yeast infections. They can offer guidance on prevention strategies and provide steps to take if the infections recur. Additionally, they are available to address any concerns or questions you may have, ensuring you have a comprehensive understanding of your condition.
Importance of Proper Postoperative Care
Following a hysterectomy, it is essential to adhere to appropriate postoperative care instructions to minimize the risk of infection, including yeast infections. Here are some important tips to remember:

1. Adhere to Wound Care Guidelines: If you have undergone an abdominal incision, diligently follow the wound care instructions provided by your healthcare provider. This will facilitate proper healing and help prevent infection.
2. Avoid Vaginal Douching: Douching disrupts the natural balance of bacteria in the vagina and can increase the risk of yeast overgrowth. It’s best to avoid this practice altogether.
3. Maintain Good Hygiene: Practice good hygiene by gently washing the external genital area with mild soap and water. Avoid using harsh soaps or cleansers that may irritate the delicate vaginal tissues.
4. Use Antibiotics Judiciously: If your healthcare provider prescribes antibiotics for postoperative care or other reasons, take them as directed. However, be aware that antibiotics can disrupt the natural vaginal flora, potentially leading to yeast infections.
5. Stay Hydrated and Follow a Healthy Diet: Drinking plenty of water and maintaining a balanced diet can support overall vaginal health and reduce the risk of infections.
When to Seek Medical Attention
While yeast infections are generally not considered serious, there are instances when it’s essential to seek medical attention. Contact your healthcare provider if:
1. Your symptoms worsen or persist despite self-care measures or over-the-counter treatments.
2. You develop new symptoms or experience unusual vaginal discharge, particularly if it is accompanied by a foul odor or changes in color.
3. If you experience recurrent yeast infections, defined as having more than four infections in a year, it is important to consult with your healthcare provider.
4. If you have a weakened immune system due to conditions like HIV/AIDS or are currently undergoing cancer treatments, seeking guidance from your healthcare provider is crucial.
Always keep in mind that your healthcare provider is the optimal resource for diagnosing and managing yeast infections. They can offer personalized guidance based on your specific situation, ensuring the most effective care and management of your condition.
Conclusion
While yeast infections can develop after a hysterectomy, they can be effectively managed through proper understanding, preventative measures, and timely treatment. By being aware of potential risks and symptoms, practicing good postoperative care, and seeking medical attention when necessary, you can prioritize your vaginal health and overall well-being. Remember that your healthcare provider is there to support you throughout your journey and provide the best possible care. Stay informed, prioritize self-care, and do not hesitate to seek professional guidance when needed.
FAQs
Can a yeast infection after hysterectomy be related to other vaginal conditions?
Yes, a yeast infection after a hysterectomy can sometimes be associated with other vaginal conditions such as bacterial vaginosis (BV) or urinary tract infections. It’s important to consult a healthcare provider for a proper diagnosis and have the appropriate treatment in this case.
Can a yeast infection after a hysterectomy cause itching outside of the vagina?
Yes, a yeast infection can cause itching not only inside the vagina but also in the surrounding vulva and perineal area.
Are menopausal symptoms and medical procedures related to yeast infections after a hysterectomy?
Menopausal symptoms and medical procedures, such as the use of hormone replacement therapy or antibiotics, can potentially increase the risk of yeast infections after a hysterectomy.
Can the use of certain products like condoms or deodorants contribute to yeast infections after a hysterectomy?
Yes, the use of certain products such as condoms or deodorants in the vaginal area can disrupt the natural balance of the vaginal microbiota and increase the risk of yeast infections.
Will a yeast infection after a hysterectomy go away without treatment?
Yeast infections typically require treatment to resolve. It is recommended to see your doctor for proper diagnosis and appropriate treatment.
Are there any bacteria that normally live in the vagina that can cause problems after a hysterectomy?
Yes, certain bacteria normally present in the vagina can become overgrown or imbalanced after a hysterectomy, potentially leading to infections such as bacterial vaginosis or yeast infections.
What are some common post-op symptoms after a hysterectomy that can be mistaken for a yeast infection?
Common post-operative symptoms after a hysterectomy, such as vaginal dryness, soreness, and discomfort around the vaginal opening, can sometimes be mistaken for a yeast infection. It is important to consult a healthcare provider for proper evaluation and diagnosis.
Can a vaginal yeast infection post-hysterectomy lead to an ovarian infection?
While it is possible for a yeast infection to occur after a hysterectomy, it is highly unlikely for it to directly lead to an ovary infection. Yeast infections primarily affect the vaginal and vulvar areas caused by an overgrowth of Candida fungus. The infection is generally localized to the reproductive organs in the lower part of the female reproductive tract.